Mahayosnand P. Gheno G. Sabra Z. Sabra D. Muslim-majority countries have fewer COVID-19 cases and deaths: a cross-country analysis of 165 countries during the 3 global peak dates in 2020-2021. HPHR. 2021;48. 10.54111/0001/vv2
To determine the difference in the total number of COVID-19 cases and deaths between Muslim-majority and non-Muslim countries, and investigate reasons for anydisparities.
A cross-country panel analysis of the total number of new COVID-19 cases per million for 165 countries was conducted from May 1, 2020 to July 1, 2021. Regression models of the total number of COVID-19 cases and deaths per million were created for the 3 global peak dates of July 31, 2020 and January 7 and April 29, 2021.
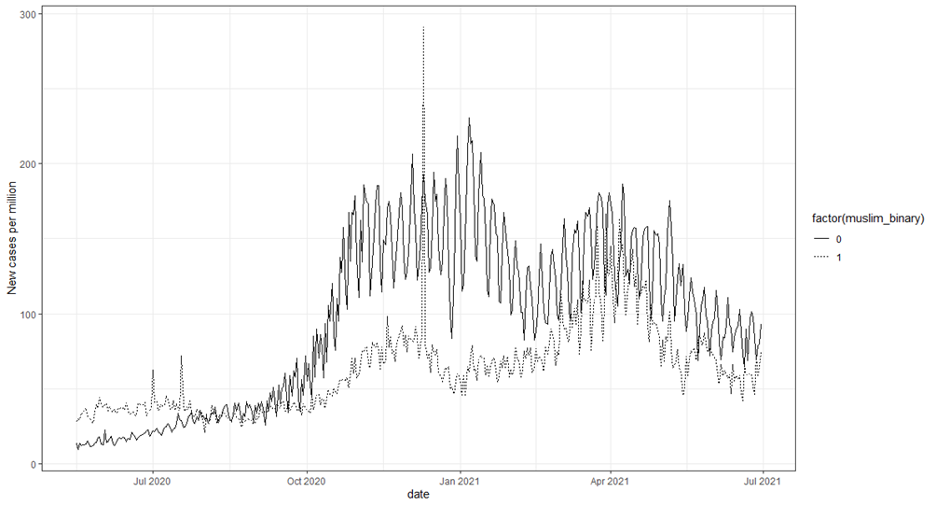
The number of daily new COVID-19 cases per million was signficantly less in Muslim-majority countries (N = 49) than non-Muslim countries (N=116), SD 1.57E-1, p-value <0.001 from May 1, 2020 to July 1, 2021. Total number of cases per million of Muslim-majority countries was significantly less on July 31st: 0.089, p-value <0.001; January 7th: SD 0.012, p-value 0.04; April 29th: SD 0.009, p-value <0.01. Total number of deaths per million of Muslim-majority countries was also significantly less on July 31st: 0.510, p-value 0.009; January 7th: SD 0.090, p-value <0.001; April 29th: SD 0.065, p-value 0.03.
The data suggests a relationship between Islamic practices and the incidence of COVID-19 and COVID-19 related deaths. This study explored how that Muslims’ practice of tahara (purity or cleanliness) is similar to many COVID-19 containment measures and tawakkul (trust in Allah) helps them remain resilient and hopeful during difficult unpredictable times, such as living through a pandemic.
It is hoped that this paper brings awareness to the positive practices of the Islamic faith as it relates to COVID-19, and to population and individual health. Research should be conducted with Muslims in Muslim-majority and non-Muslim countries to further study the relationship between Islam and health.
The objective of this research was to determine if there was a difference in the total number of COVID-19 cases and deaths per million between Muslim-majority (N=49)and non-Muslim countries (M=116), and to investigate possible explanations for any disparities.
Healthcare systems are reported to be corrupt, limited, or under-resourced in LMIC (low- and middle-income countries).1 With limited healthcare resources and poor living conditions, it was believed that LMICwere more vulnerable to COVID-19. In regards to combating COVID-19, LMICs average 1-10 SAO (surgeons, anesthesiologists, and obstetricians) per 100,000 compared to the estimated need of 20 SAO per 100,000.2 It is estimated that LMICs have 0.1-2.5 ICU beds per 100,000 while higher-income countries have 5-30 in.
In Bangladesh, a Muslim-majority country, full lockdown was nearly impossible as there was a strong association between loss of livelihood and an increased unemployment rate due to full business shutdown.3 Partial lockdown with social distancing and multi-sectoral (health, economy, agriculture, food, etc.) collaboration was recommended. Identifying and isolating active COVID-19 cases, rapid testing, and contact tracing were found to be extremely difficult for under-resourced LMICs. In LMIC, a percentage of the population is dependent on daily wages (meaning funds are sufficient for only a day’s worth of food) both in the rural and urban settings.4 In the slums of India, a non-Muslim country, if people did not go to work, they had a high likelihood of losing their jobs. For individuals living in these situations, following social distancing or lockdown directives meant weighing the potential risks of COVID-19 versus the immediate risk of hunger.5 If governments want this population to stay home in hopes of reducing the spread of COVID-19, they must provide them daily income and necessary resources in order to survive.
LMIC currently in war and crisis face more imminent death and destruction as shown in the following examples of Muslim-majority countries: Afghanistan had trouble managing its wounded citizens, and Yemen faced daily airstrikes and the reemergence of diseases such as cholera, diarrhea, dengue, and measles.6,7 Both reports stressed that the United Nations should pressure for ceasefires to combat the expansion of COVID-19, while also lifting blockades in Gaza toallow the transit of much-needed healthcare aid and assistance.8Certain measures were conducive to possibly containing the spread of COVID-19. For example, due to Gaza’s land, air and water blockade, its borders were mostly closed during the early months of the outbreak which prevented travelers and foreigners from entering.9 Border quarantine and isolation of positive COVID-19 cases was said to inhibit the proliferation of the pandemic.
Two methods reported to help contain COVID-19 in LMIC were found to be: (1) public education and community outreach, and (2) pragmatic multi-sectoral (health, business, schools, agricultural, etc.) collaboration in adhering to amended WHO COVID-19 guidelines after individual countries weighed the ethical and economical risks against their health and social benefits.10 Beneficial counseling included canceling elective medical procedures, seeking only emergency medical care, self-isolating if sick, and allocating limited PPE (personal protective equipment) usage for healthcare professionals. Appropriating resources for telepsychiatry services for the growing need during this pandemic was continuously recommended.2
Growing objective scientific research suggests religious faith is an important resource for health and well-being and benefits the “immune functioning and vulnerability to infection.”11 Quoting various religions including Islam, Koenig stressed the importance of maintaining spiritual, mental, and physical resilience during the COVID-19 pandemic. Religious beliefs and practices helped individuals in their abilities to cope with disease, recover from hospitalization, and have positive attitudes.11 An Italian study showed that more severe COVID-19 affectees reported higher religious behavior and that Google searches across 95 countries for topics related to prayer increased during the pandemic.12
Hand hygiene among health care workers was analyzed across eight religions.13 Islam was one of three religions that had precise rules for handwashing specified in sacred texts. Islam and two other religions emphasized the importance of cleanliness and personal hygiene. Their followers were encouraged to adhere to daily hygienic practices for individual, communal, and environmental benefits.
Litman et al. suggested that individuals with both intrinsic and extrinsic religious motivation to maintain high levels of cleanliness were more interested in staying clean to remain physically and religiously cleansed.14 Litman recommended that further research be conducted to examine if enhanced religious cleanliness would translate into actual health benefits, such as reduced incidence of infectious diseases or food-borne illnesses.
This study focused on the confirmed COVID-19 numbers of cases and deaths per million population in 165 countries. Data was obtained from publicly compiled resources that are updated daily throughout the world.15 To address possible contributing factors, the following variables were also compiled: stringency, population density, GDP, and vaccinated per hundred.Muslim-majority countries (N=49) had more than 50.0% Muslims (50.7 – 100%) with an average of 87.5% Muslim population.16 Non-Muslim countries (N=116) consisted of countries with less than 49.6% Muslims (49.6 – 0%) with an average of 6.6% Muslim population. [See Table 1] .
| Country | Percentage of Muslim population | Muslim_binary: 0 = Non-Muslim 1 = Muslim-majority | LMIC classification | Freedom Category |
1 | Bolivia | 0 | 0 | Lower middle income | Partly Free |
2 | Chile | 0 | 0 | High income | Free |
3 | Costa Rica | 0 | 0 | Upper middle income | Free |
4 | Dominican Republic | 0 | 0 | Upper middle income | Partly Free |
5 | Ecuador | 0 | 0 | Upper middle income | Partly Free |
6 | El Salvador | 0 | 0 | Lower middle income | Partly Free |
7 | Estonia | 0 | 0 | High income | Free |
8 | Guatemala | 0 | 0 | Upper middle income | Partly Free |
9 | Haiti | 0 | 0 | Lower middle income | Partly Free |
10 | Laos | 0 | 0 | Lower middle income | Not Free |
11 | Nicaragua | 0 | 0 | Lower middle income | Not Free |
12 | Papua New Guinea | 0 | 0 | Lower middle income | Partly Free |
13 | Paraguay | 0 | 0 | Upper middle income | Partly Free |
14 | Peru | 0 | 0 | Upper middle income | Partly Free |
15 | Uruguay | 0 | 0 | High income | Free |
16 | Mexico | 0.01 | 0 | Upper middle income | Partly Free |
17 | Poland | 0.02 | 0 | High income | Free |
18 | Bahamas | 0.1 | 0 | High income | Free |
19 | Cuba | 0.1 | 0 | Upper middle income | Not Free |
20 | Japan | 0.1 | 0 | High income | Free |
21 | Lesotho | 0.1 | 0 | Lower middle income | Partly Free |
22 | Lithuania | 0.1 | 0 | High income | Free |
23 | South Korea | 0.1 | 0 | High income | Free |
24 | Timor | 0.1 | 0 | Lower middle income | Free |
25 | Vietnam | 0.1 | 0 | Lower middle income | Not Free |
26 | Czechia | 0.15 | 0 | High income | Free |
27 | Latvia | 0.15 | 0 | High income | Free |
28 | Slovakia | 0.15 | 0 | High income | Free |
29 | Belize | 0.2 | 0 | Lower middle income | Free |
30 | Bhutan | 0.2 | 0 | Lower middle income | Partly Free |
31 | Colombia | 0.2 | 0 | Upper middle income | Partly Free |
32 | Dominica | 0.2 | 0 | Upper middle income | Free |
33 | Iceland | 0.2 | 0 | High income | Free |
34 | Jamaica | 0.2 | 0 | Upper middle income | Free |
35 | Angola | 0.3 | 0 | Lower middle income | Not Free |
36 | Honduras | 0.3 | 0 | Lower middle income | Partly Free |
37 | Brazil | 0.36 | 0 | Upper middle income | Free |
38 | Botswana | 0.4 | 0 | Upper middle income | Free |
39 | Moldova | 0.4 | 0 | Upper middle income | Partly Free |
40 | Namibia | 0.4 | 0 | Upper middle income | Free |
41 | Portugal | 0.4 | 0 | High income | Free |
42 | Venezuela | 0.4 | 0 | Lower middle income | Not Free |
43 | Hungary | 0.5 | 0 | High income | Partly Free |
44 | Romania | 0.65 | 0 | Upper middle income | Free |
45 | Panama | 0.7 | 0 | Upper middle income | Free |
46 | Zimbabwe | 0.7 | 0 | Lower middle income | Not Free |
47 | Belarus | 0.75 | 0 | Upper middle income | Not Free |
48 | Argentina | 0.9 | 0 | Upper middle income | Free |
49 | New Zealand | 0.9 | 0 | High income | Free |
50 | Zambia | 1 | 0 | Lower middle income | Partly Free |
51 | Seychelles | 1.1 | 0 | High income | Free |
52 | United States | 1.1 | 0 | High income | Free |
53 | Ireland | 1.4 | 0 | High income | Free |
54 | Barbados | 1.5 | 0 | High income | Free |
55 | Croatia | 1.5 | 0 | High income | Free |
56 | Ukraine | 1.7 | 0 | Lower middle income | Partly Free |
57 | China | 1.725 | 0 | Upper middle income | Not Free |
58 | Cambodia | 1.9 | 0 | Lower middle income | Not Free |
59 | South Africa | 1.9 | 0 | Upper middle income | Free |
60 | Cape Verde | 2 | 0 | Lower middle income | Free |
61 | Congo | 2 | 0 | Lower middle income | Not Free |
62 | Andorra | 2.6 | 0 | High income | Free |
63 | Australia | 2.6 | 0 | High income | Free |
64 | Malta | 2.6 | 0 | High income | Free |
65 | Spain | 2.6 | 0 | High income | Free |
66 | Finland | 2.7 | 0 | High income | Free |
67 | Luxembourg | 3 | 0 | High income | Free |
68 | Serbia | 3.1 | 0 | Upper middle income | Partly Free |
69 | Canada | 3.2 | 0 | High income | Free |
70 | Slovenia | 3.6 | 0 | High income | Free |
71 | Nepal | 4.2 | 0 | Lower middle income | Partly Free |
72 | Myanmar | 4.3 | 0 | Lower middle income | Not Free |
73 | Thailand | 4.3 | 0 | Upper middle income | Not Free |
74 | Italy | 4.8 | 0 | High income | Free |
75 | Rwanda | 4.8 | 0 | Low income | Not Free |
76 | Mongolia | 5 | 0 | Lower middle income | Free |
77 | Netherlands | 5.1 | 0 | High income | Free |
78 | Switzerland | 5.2 | 0 | High income | Free |
79 | Denmark | 5.4 | 0 | High income | Free |
80 | Germany | 5.7 | 0 | High income | Free |
81 | Greece | 5.7 | 0 | High income | Free |
82 | Norway | 5.7 | 0 | High income | Free |
83 | Trinidad and Tobago | 5.8 | 0 | High income | Free |
84 | Fiji | 6.3 | 0 | Upper middle income | Partly Free |
85 | United Kingdom | 6.3 | 0 | High income | Free |
86 | Guyana | 7.3 | 0 | Upper middle income | Free |
87 | Belgium | 7.6 | 0 | High income | Free |
88 | Austria | 8 | 0 | High income | Free |
89 | Philippines | 8 | 0 | Lower middle income | Partly Free |
90 | Sweden | 8.1 | 0 | High income | Free |
91 | France | 8.8 | 0 | High income | Free |
92 | Sri Lanka | 9.7 | 0 | Lower middle income | Partly Free |
93 | Burundi | 10 | 0 | Low income | Not Free |
94 | Democratic Republic of Congo | 10 | 0 | Low income | Not Free |
95 | Eswatini | 10 | 0 | Lower middle income | Not Free |
96 | Gabon | 10 | 0 | Upper middle income | Not Free |
97 | Madagascar | 10 | 0 | Low income | Partly Free |
98 | Georgia | 10.7 | 0 | Upper middle income | Partly Free |
99 | Kenya | 11.2 | 0 | Lower middle income | Partly Free |
100 | Bulgaria | 13.4 | 0 | Upper middle income | Free |
101 | Russia | 13.5 | 0 | Upper middle income | Not Free |
102 | Suriname | 13.9 | 0 | Upper middle income | Free |
103 | Uganda | 14 | 0 | Low income | Not Free |
104 | India | 14.2 | 0 | Lower middle income | Partly Free |
105 | Singapore | 14.7 | 0 | High income | Partly Free |
106 | Central African Republic | 15 | 0 | Low income | Not Free |
107 | Mauritius | 17.3 | 0 | Upper middle income | Free |
108 | Mozambique | 17.9 | 0 | Low income | Partly Free |
109 | Ghana | 18 | 0 | Lower middle income | Free |
110 | Israel | 18 | 0 | High income | Free |
111 | Liberia | 20 | 0 | Low income | Partly Free |
112 | Malawi | 20 | 0 | Low income | Partly Free |
113 | South Sudan | 20 | 0 | Low income | Not Free |
114 | Togo | 20 | 0 | Low income | Partly Free |
115 | Benin | 27.7 | 0 | Lower middle income | Partly Free |
116 | Cyprus | 28.2 | 0 | High income | Free |
117 | Cameroon | 30 | 0 | Lower middle income | Not Free |
118 | Ethiopia | 33.9 | 0 | Low income | Not Free |
119 | Tanzania | 35.2 | 0 | Lower middle income | Partly Free |
120 | Cote d’Ivoire | 42.9 | 0 | Lower middle income | Partly Free |
121 | Eritrea | 43.8 | 0 | Low income | Not Free |
122 | Nigeria | 49.6 | 0 | Lower middle income | Partly Free |
123 | Bosnia and Herzegovina | 50.7 | 1 | Upper middle income | Partly Free |
124 | Lebanon | 57.7 | 1 | Upper middle income | Partly Free |
125 | Chad | 58 | 1 | Low income | Not Free |
126 | Albania | 58.8 | 1 | Upper middle income | Partly Free |
127 | Malaysia | 61.3 | 1 | Upper middle income | Partly Free |
128 | Burkina Faso | 61.5 | 1 | Low income | Partly Free |
129 | Kazakhstan | 70.2 | 1 | Upper middle income | Not Free |
130 | Bahrain | 73.7 | 1 | High income | Not Free |
131 | Kuwait | 74.6 | 1 | High income | Partly Free |
132 | United Arab Emirates | 76 | 1 | High income | Not Free |
133 | Qatar | 77.5 | 1 | High income | Not Free |
134 | Sierra Leone | 78.6 | 1 | Low income | Partly Free |
135 | Brunei | 78.8 | 1 | High income | Not Free |
136 | Kyrgyzstan | 80 | 1 | Lower middle income | Not Free |
137 | Oman | 85.9 | 1 | High income | Not Free |
138 | Indonesia | 87.2 | 1 | Lower middle income | Partly Free |
139 | Guinea | 89.1 | 1 | Low income | Partly Free |
140 | Bangladesh | 90.4 | 1 | Lower middle income | Partly Free |
141 | Egypt | 92.35 | 1 | Lower middle income | Not Free |
142 | Mali | 95 | 1 | Low income | Not Free |
143 | Gambia | 95.7 | 1 | Low income | Partly Free |
144 | Iraq | 95.7 | 1 | Upper middle income | Not Free |
145 | Senegal | 96.1 | 1 | Lower middle income | Partly Free |
146 | Pakistan | 96.5 | 1 | Lower middle income | Partly Free |
147 | Uzbekistan | 96.5 | 1 | Lower middle income | Not Free |
148 | Tajikistan | 96.7 | 1 | Lower middle income | Not Free |
149 | Azerbaijan | 96.9 | 1 | Upper middle income | Not Free |
150 | Djibouti | 97 | 1 | Lower middle income | Not Free |
151 | Libya | 97 | 1 | Upper middle income | Not Free |
152 | Sudan | 97 | 1 | Low income | Not Free |
153 | Saudi Arabia | 97.1 | 1 | High income | Not Free |
155 | Jordan | 97.2 | 1 | Upper middle income | Not Free |
155 | Palestine | 97.5 | 1 | Lower middle income | Not Free |
156 | Niger | 98.3 | 1 | Low income | Partly Free |
157 | Algeria | 99 | 1 | Lower middle income | Not Free |
158 | Morocco | 99 | 1 | Lower middle income | Partly Free |
159 | Yemen | 99.1 | 1 | Low income | Not Free |
160 | Turkey | 99.2 | 1 | Upper middle income | Not Free |
161 | Iran | 99.4 | 1 | Lower middle income | Not Free |
162 | Afghanistan | 99.6 | 1 | Low income | Not Free |
163 | Somalia | 99.8 | 1 | Low income | Not Free |
164 | Tunisia | 99.8 | 1 | Lower middle income | Free |
165 | Mauritania | 100 | 1 | Lower middle income | Partly Free |
Freedom scores and categories (free, partly free, and not free) were obtained by Freedom House.17 A country’s freedom score is based on the combination of the overall score of its political rights and civil liberties after being equally weighted.18 The freedom score is then used to determine its freedom category. All 49 Muslim-majoritycountries were considered “partly” or “not free”.17 Countries were further categorized as low- lower-middle- upper-middle- and high-income countries.19
A cross-country panel analysis of the total number of new COVID-19 cases for 165 countries was conducted from May 1, 2020 to July 1, 2021. Control variables included stringency index at t-15 and t-5, and low- lower-middle- and upper-middle-income. Regression models of the 165 countries were created for the 3 global COVID-19 peak dates of January 7 and July 31, 2020, and April 29, 2021 to analyze the total number of COVID-19 cases and deaths per million. Control variables included vaccinated per hundred, population density, low- low-middle- and upper-middle-income, whether a country is free or partly free, and GDP per capita.
The number of daily new COVID-19 cases per million was signficantly less in Muslim-majority countries (N = 49) compared to non-Muslim countries (N=116), SD 1.57E-1, p-value <0.001, controling for stringency index at t-15 and t-5, low- lower-middle- and upper-middle-income of a country. (See Table 2).
Table 2
Dependent variable: new daily cases | ||||
| estimate | std.error | p.value |
|
Control variables |
|
|
|
|
Stringency index at t-15 | -0.028 | 0.003 | 0 | *** |
Stringency index at t-5 | 0.050 | 0.003 | 0 | *** |
Low income | -3.805 | 1.93E-19 | 0 | *** |
Lower middle income | -1.697 | 1.77E-17 | 0 | *** |
Upper middle income | -0.543 | 1.1E-17 | 0 | *** |
Variable of interest |
|
|
|
|
Muslim | -0.048 | 1.57E-17 | 0 | *** |
Signif. codes: 0 ‘***’ 0.001 ‘**’ 0.01 ‘*’ 0.05 ‘.’ 0.1 ‘ ’ 1
Total number of cases per million of Muslim-majority countries was significantly less than non-Muslim countries in the 3 peak dates controling for vaccinated per hundred, population density, low- lower-middle- and upper-middle-income, being not or partly free, and GDP per capita. July 31, 2020: 0.089, p-value <0.001 (See Table 3), January 7, 2021: SD 0.012, p-value 0.04 (See Table 4), April 29, 2021: SD 0.009, p-value <0.01 (see Table 5),
Table 3
Dependent variable: total cases, day: July 31, 2020 | ||||||||
| Model 1 | Model 2 | ||||||
term | estimate | std.error | p.value |
| estimate | std.error | p.value |
|
(Intercept) | 7.796 | 0.004 | 0 | *** | 7.614 | 0.005 | 0 | *** |
Control variables |
|
|
|
|
|
|
|
|
Vaccinated per hundred |
|
|
|
|
|
|
|
|
Population density | -7.73E-05 | 7.85E-07 | 0 | *** | -7.4E-05 | 8.69E-07 | 0 | *** |
Low income | -3.328 | 0.014 | 0 | *** | -2.196 | 0.021 | 0 | *** |
Lower middle income | -1.568 | 0.006 | 0 | *** | -0.858 | 0.008 | 0 | *** |
Upper middle income | -0.429 | 0.005 | 0 | *** | 0.468 | 0.006 | 0 | *** |
Not Free | 0.979 | 0.004 | 0 | *** | -0.370 | 0.008 | 0 | *** |
Partly Free | 0.766 | 0.005 | 0 | *** | 0.225 | 0.005 | 0 | *** |
GDP per capita | 1.38E-05 | 7.62E-08 | 0 | *** | 1.43E-05 | 8.95E-08 | 0 | *** |
Interaction: Muslim, Vaccinated per hundred |
|
|
|
|
|
|
|
|
Interaction: Muslim, Population density |
|
|
|
| 0.001 | 4.44E-06 | 0 | *** |
Interaction: Muslim, Low income |
|
|
|
| -0.845 | 0.029 | 0 | *** |
Interaction: Muslim, Lower middle income |
|
|
|
| -0.246 | 0.013 | 0 | *** |
Interaction: Muslim, Upper middle income |
|
|
|
| -1.392 | 0.011 | 0 | *** |
Interaction: Muslim, Not Free |
|
|
|
| 2.986 | 0.087 | 0 | *** |
Interaction: Muslim, Partly Free |
|
|
|
| 2.239 | 0.088 | 0 | *** |
Interaction: Muslim, GDP per capita |
|
|
|
| 1.08E-05 | 1.91E-07 | 0 | *** |
Variable of interest |
|
|
|
|
|
|
|
|
Muslim |
|
|
|
| -1.761 | 0.089 | 0 | *** |
Statistics |
|
|
|
|
|
|
|
|
AIC | 1,889,724 | 1,758,959 | ||||||
Signif. codes: 0 ‘***’ 0.001 ‘**’ 0.01 ‘*’ 0.05 ‘.’ 0.1 ‘ ’ 1
Table 4
Dependent variable: total cases, day: January 07, 2021 | ||||||||
| Model 1 | Model 2 | ||||||
term | estimate | std.error | p.value |
| estimate | std.error | p.value |
|
(Intercept) | 10.153 | 0.002 | 0 | *** | 10.132 | 0.002 | 0 | *** |
Control variables |
|
|
|
|
|
|
|
|
Vaccinated per hundred | 0.035 | 2.00E-04 | 0 | *** | 0.031 | 2.00E-04 | 0 | *** |
Population density | -5.80E-05 | 3.72E-07 | 0 | *** | -6.8E-05 | 3.98E-07 | 0 | *** |
Low income | -3.675 | 0.009 | 0 | *** | -3.336 | 0.012 | 0 | *** |
Lower middle income | -1.455 | 0.003 | 0 | *** | -1.430 | 0.003 | 0 | *** |
Upper middle income | -0.203 | 0.002 | 0 | *** | -0.140 | 0.002 | 0 | *** |
Not Free | -0.305 | 0.002 | 0 | *** | -1.038 | 0.004 | 0 | *** |
Partly Free | 0.025 | 0.002 | 0 | *** | 0.005 | 0.002 | 0.03 | * |
GDP per capita | 6.04E-06 | 3.26E-08 | 0 | *** | 6.4E-06 | 3.37E-08 | 0 | *** |
Interaction: Muslim, Vaccinated per hundred |
|
|
|
| -0.123 | 0.003 | 0 | *** |
Interaction: Muslim, Population density |
|
|
|
| 0.001 | 6.56E-06 | 0 | *** |
Interaction: Muslim, Low income |
|
|
|
| 0.320 | 0.018 | 0 | *** |
Interaction: Muslim, Lower middle income |
|
|
|
| 0.666 | 0.008 | 0 | *** |
Interaction: Muslim, Upper middle income |
|
|
|
| 0.581 | 0.006 | 0 | *** |
Interaction: Muslim, Not Free |
|
|
|
| 0.248 | 0.010 | 0 | *** |
Interaction: Muslim, Partly Free |
|
|
|
| -0.840 | 0.010 | 0 | *** |
Interaction: Muslim, GDP per capita |
|
|
|
| 1.03E-05 | 1.46E-07 | 0 | *** |
Variable of interest |
|
|
|
|
|
|
|
|
Muslim |
|
|
|
| -0.024 | 0.012 | 0.04 | * |
Statistics |
|
|
|
|
|
|
|
|
AIC | 2,963,844 | 2,704,589 | ||||||
Signif. codes: 0 ‘***’ 0.001 ‘**’ 0.01 ‘*’ 0.05 ‘.’ 0.1 ‘ ’ 1
Table 5
Dependent variable: total cases ; day: April 29, 2021 | ||||||||
| Model 1 | Model 2 | ||||||
term | estimate | std.error | p.value |
| estimate | std.error | p.value |
|
(Intercept) | 10.788 | 0.001 | 0 | *** | 10.809 | 0.001 | 0 | *** |
Control variables |
|
|
|
|
|
|
|
|
Vaccinated per hundred | 0.013 | 3.41E-05 | 0 | *** | 0.012 | 3.65E-05 | 0 | *** |
Population density | -3.09E-05 | 2.69E-07 | 0 | *** | -3.8E-05 | 2.86E-07 | 0 | *** |
Low income | -3.628 | 0.006 | 0 | *** | -3.199 | 0.008 | 0 | *** |
Lower middle income | -1.564 | 0.002 | 0 | *** | -1.586 | 0.002 | 0 | *** |
Upper middle income | -0.282 | 0.001 | 0 | *** | -0.324 | 0.002 | 0 | *** |
Not Free | -0.330 | 0.001 | 0 | *** | -0.981 | 0.003 | 0 | *** |
Partly Free | -0.003 | 0.001 | 0.01 | * | -0.025 | 0.002 | 0 | *** |
GDP per capita | 1.14E-06 | 2.55E-08 | 0 | *** | 1.43E-06 | 2.63E-08 | 0 | *** |
Interaction: Muslim, Vaccinated per hundred |
|
|
|
| 0.011 | 0.001 | 0 | *** |
Interaction: Muslim, Population density |
|
|
|
| 0.001 | 2.48E-06 | 0 | *** |
Interaction: Muslim, Low income |
|
|
|
| 0.390 | 0.013 | 0 | *** |
Interaction: Muslim, Lower middle income |
|
|
|
| 1.097 | 0.006 | 0 | *** |
Interaction: Muslim, Upper middle income |
|
|
|
| 1.189 | 0.005 | 0 | *** |
Interaction: Muslim, Not Free |
|
|
|
| -0.003 | 0.008 | 0.68 |
|
Interaction: Muslim, Partly Free |
|
|
|
| -0.874 | 0.007 | 0 | *** |
Interaction: Muslim, GDP per capita |
|
|
|
| 1.17E-05 | 1.18E-07 | 0 | *** |
Variable of interest |
|
|
|
|
|
|
|
|
Muslim |
|
|
|
| -0.301 | 0.009 | 0 | *** |
Statistics |
|
|
|
|
|
|
|
|
AIC | 525,969 | 433,350 | ||||||
Signif. codes: 0 ‘***’ 0.001 ‘**’ 0.01 ‘*’ 0.05 ‘.’ 0.1 ‘ ’ 1
Total number of deaths per million of Muslim-majority countries was significantly less than non-Muslim countries in the 3 peak dates controling for the same variables as above. July 31, 2020: 0.510, p-value 0.009 (See Table 6); January 7, 2021: SD 0.090, p-value <0.001 (See Table 7), April 29, 2021: SD 0.065, p-value 0.03 (See Table 8).
Table 6
Dependent variable: total deaths; day: July 31, 2020 | ||||||||
| Model 1 | Model 2 | ||||||
term | estimate | std.error | p.value |
| estimate | std.error | p.value |
|
(Intercept) | 3.025 | 0.098 | 0 | *** | 1.375 | 0.109 | 0 | *** |
Control variables |
|
|
|
|
|
|
|
|
Vaccinated per hundred |
|
|
|
|
|
|
|
|
Total cases per million | 1.32E-04
| 1.65E-06 | 0 | *** | 1.78E-04 | 2.04E-06 | 0 | *** |
Population density | -4.93E-04 | 3.43E-05 | 0 | *** | -4.8E-04 | 2.72E-05 | 0 | *** |
Low income | -0.641 | 0.107 | 0 | *** | -0.474 | 0.165 | 0.004 | ** |
Lower middle income | 0.319 | 0.058 | 0 | *** | 0.259 | 0.066 | 0 | *** |
Upper middle income | 0.688 | 0.035 | 0 | *** | 0.631 | 0.039 | 0 | *** |
Not Free | -0.266 | 0.035 | 0 | *** | -0.714 | 0.066 | 0 | *** |
Partly Free | 0.692 | 0.027 | 0 | *** | 1.159 | 0.031 | 0 | *** |
GDP per capita | -6.02E-06 | 4.90E-07 | 0 | *** | -9.8E-07 | 4.58E-07 | 0.032 | * |
Median age | 0.092 | 0.002 | 0 | *** | 0.112 | 0.002 | 0 | *** |
Cardiovasc death rate | -0.006 | 1.16E-04 | 0 | *** | -0.005 | 1.18E-04 | 0 | *** |
Diabetes prevalence | -0.170 | 0.004 | 0 | *** | -0.130 | 0.005 | 0 | *** |
Interaction: Muslim, Vaccinated per hundred |
|
|
|
|
|
|
|
|
Interaction: Muslim, Total cases per million |
|
|
|
| -1.5E-04 | 4.07E-06 | 0 | *** |
Interaction: Muslim, Population density |
|
|
|
| 2.56E-04 | 6.97E-05 | 0 | *** |
Interaction: Muslim, Low income |
|
|
|
| 0.121 | 0.204 | 0.553 |
|
Interaction: Muslim, Lower middle income |
|
|
|
| 0.292 | 0.107 | 0.006 | ** |
Interaction: Muslim, Upper middle income |
|
|
|
| -0.446 | 0.098 | 0 | *** |
Interaction: Muslim, Not Free |
|
|
|
| 4.128 | 0.506 | 0 | *** |
Interaction: Muslim, Partly Free |
|
|
|
| 1.265 | 0.504 | 0.012 | * |
Variable of interest |
|
|
|
|
|
|
|
|
Muslim |
|
|
|
| -1.322 | 0.510 | 0.009 | ** |
Statistics |
|
|
|
|
|
|
|
|
AIC | 12,146 | 8,632 | ||||||
|
|
| ||||||
Signif. codes: 0 ‘***’ 0.001 ‘**’ 0.01 ‘*’ 0.05 ‘.’ 0.1 ‘ ’ 1
Table 7
Dependent variable: total deaths; day: January 7, 2021 | ||||||||
| Model 1 | Model 2 | ||||||
term | estimate | std.error | p.value |
| estimate | std.error | p.value |
|
(Intercept) | 4.587 | 0.045 | 0 | *** | 4.315 | 0.050 | 0 | *** |
Control variables |
|
|
|
|
|
|
|
|
Vaccinated per hundred | 0.007 | 0.002 | 0.001 | *** | 0.015 | 0.002 | 0 | *** |
Total cases per million | 2.3E-05 | 1.97E-07 | 0 | *** | 2.11E-05 | 2.05E-07 | 0 | *** |
Population density | -5.66E-04 | 2.53E-05 | 0 | *** | -7.1E-04 | 3.51E-05 | 0 | *** |
Low income | -1.814 | 0.064 | 0 | *** | -1.884 | 0.103 | 0 | *** |
Lower middle income | -0.063 | 0.027 | 0.02 | * | -0.062 | 0.032 | 0.06 | ° |
Upper middle income | 0.560 | 0.017 | 0 | *** | 0.671 | 0.020 | 0 | *** |
Not Free | -0.316 | 0.018 | 0 | *** | -1.225 | 0.033 | 0 | *** |
Partly Free | 0.351 | 0.014 | 0 | *** | 0.477 | 0.015 | 0 | *** |
GDP per capita | -6.57E-06 | 2.9E-07 | 0 | *** | -6.8E-06 | 2.97E-07 | 0 | *** |
Median age | 0.045 | 0.001 | 0 | *** | 0.058 | 0.001 | 0 | *** |
Cardiovasc death rate | -0.002 | 5.16E-05 | 0 | *** | -0.003 | 5.36E-05 | 0 | *** |
Diabetes prevalence | -0.042 | 0.002 | 0 | *** | -0.056 | 0.002 | 0 | *** |
Interaction: Muslim, Vaccinated per hundred |
|
|
|
| 0.118 | 0.036 | 0.001 | ** |
Interaction: Muslim, Total cases per million |
|
|
|
| 3.37E-05 | 1.55E-06 | 0 | *** |
Interaction: Muslim, Population density |
|
|
|
| -2.6E-04 | 8.33E-05 | 0.002 | ** |
Interaction: Muslim, Low income |
|
|
|
| 1.849 | 0.137 | 0 | *** |
Interaction: Muslim, Lower middle income |
|
|
|
| 1.337 | 0.067 | 0 | *** |
Interaction: Muslim, Upper middle income |
|
|
|
| 0.418 | 0.047 | 0 | *** |
Interaction: Muslim, Not Free |
|
|
|
| 0.913 | 0.066 | 0 | *** |
Interaction: Muslim, Partly Free |
|
|
|
| -1.003 | 0.059 | 0 | *** |
Variable of interest |
|
|
|
|
|
|
|
|
Muslim |
|
|
|
| -0.624 | 0.090 | 0 | *** |
Statistics |
|
|
|
|
|
|
|
|
AIC | 26,527 | 22,898 | ||||||
Signif. codes: 0 ‘***’ 0.001 ‘**’ 0.01 ‘*’ 0.05 ‘.’ 0.1 ‘ ’ 1
Table 8
Dependent variable: total deaths; day: April 29, 2021 | ||||||||
| Model 1 | Model 2 | ||||||
term | estimate | std.error | p.value |
| estimate | std.error | p.value |
|
(Intercept) | 5.324 | 0.033 | 0 | *** | 5.128 | 0.035 | 0 | *** |
Control variables |
|
|
|
|
|
|
|
|
Vaccinated per hundred | -0.014 | 4.09E-04 | 0 | *** | -0.011 | 4.28E-04 | 0 | *** |
Total cases per million | 1.52E-05 | 1.06E-07 | 0 | *** | 1.33E-05 | 1.13E-07 | 0 | *** |
Population density | -4.45E-04 | 1.73E-05 | 0 | *** | -0.001 | 2.54E-05 | 0 | *** |
Low income | -2.052 | 0.048 | 0 | *** | -2.093 | 0.070 | 0 | *** |
Lower middle income | -0.333 | 0.020 | 0 | *** | -0.427 | 0.024 | 0 | *** |
Upper middle income | 0.397 | 0.013 | 0 | *** | 0.431 | 0.015 | 0 | *** |
Not Free | -0.409 | 0.014 | 0 | *** | -1.068 | 0.024 | 0 | *** |
Partly Free | 0.333 | 0.010 | 0 | *** | 0.479 | 0.011 | 0 | *** |
GDP per capita | -6.42E-06 | 2.31E-07 | 0 | *** | -6.7E-06 | 2.35E-07 | 0 | *** |
Median age | 0.037 | 0.001 | 0 | *** | 0.048 | 0.001 | 0 | *** |
Cardiovasc death rate | -0.002 | 3.88E-05 | 0 | *** | -0.002 | 4.03E-05 | 0 | *** |
Diabetes prevalence | -0.034 | 0.001 | 0 | *** | -0.048 | 0.002 | 0 | *** |
Interaction: Muslim, Vaccinated per hundred |
|
|
|
| -0.027 | 0.002 | 0 | *** |
Interaction: Muslim, Total cases per million |
|
|
|
| 2.15E-05 | 6.45E-07 | 0 | *** |
Interaction: Muslim, Population density |
|
|
|
| 1.3E-05 | 4.5E-05 | 0.77 |
|
Interaction: Muslim, Low income |
|
|
|
| 1.326 | 0.098 | 0 | *** |
Interaction: Muslim, Lower middle income |
|
|
|
| 0.940 | 0.050 | 0 | *** |
Interaction: Muslim, Upper middle income |
|
|
|
| -0.011 | 0.043 | 0.80 |
|
Interaction: Muslim, Not Free |
|
|
|
| 0.369 | 0.047 | 0 | *** |
Interaction: Muslim, Partly Free |
|
|
|
| -1.234 | 0.043 | 0 | *** |
Variable of interest |
|
|
|
|
|
|
|
|
Muslim |
|
|
|
| -0.142 | 0.065 | 0.03 | * |
Statistics |
|
|
|
|
|
|
|
|
AIC | 40,780 | 35,608
| ||||||
Signif. codes: 0 ‘***’ 0.001 ‘**’ 0.01 ‘*’ 0.05 ‘.’ 0.1 ‘ ’ 1
Panel data analysis was used to analyze the total number of COVID-19 cases per million for each country from May 1, 2020 to July 1, 2021. Conducting a panel data analysis helps to eliminate possible multicollinearity problems and is a good test for a time series analysis. Table 2 depicts a strong statistical difference between the 49 Muslim-majority countries (muslim_binary = 1) versus the 116 non-Muslim countries (muslim_binary = 2) during this 13-month. The one outlying date in December 2020 was due to the Muslim-majority country of Turkey having reported an extraordinary number of cases assumed to be reporting error. Regression models were made for each of the individual 3 peak dates; with one model for total number of cases per million and the other for total number of deaths per million. Choosing to study 3 distinct peak dates during the pandemic’s 3 COVID-19 waves was chosen to strengthen the argument that Muslim-majority countries have fewer cases and deaths over various moments in time.
The incidence of COVID-19 cases or COVID-19 related deaths in Muslim-majority countries can be a potential result of other contributing factors. To account for country population variation, the total number of cases and deaths per million were studied. To address other possible confounding factors of COVID-19, the following variables were added: population density, stringency, vaccinated per hundred, population density, and GDP per capita. The stringency index takes into account a country’s ability to enforce 9 possible preventive measures ranging from school or work closures, cancellation or restrictions of public gatherings; to restrictions on domestic and international travel.20 Including freedom categories was important because all 49 Muslim-majority countries are classified to be partly or not free. Therefore, determining the effects of similar countries was of interest. Last, the status of LMICwas of interest because 40/49 (82%) of the Muslim-majority countries are low- low-middle- or upper-middle-income countries, yet the remaining 9 countries are quite wealthy.
The results of this data poses an interesting global public health issue. It suggests the possibility that Muslims’ religious practices may have an impact on COVID-19 incidence. It is not to say that all citizens (Muslim or non-Muslims) in Muslim-majority countries follow prescribed practices of the Islamic faith. However, given the strong association of a possible religion and health connection is reason to explore the possibilities of this implication. This section is meant to share insights to some Islamic practices that may influence the numbers of COVID-19 cases and deaths, and a population’s health in general.
In Islam, social iolation, quarantine, and sanitation are in alignment with the WHO pandemic guidelines.21 Bentley at el showed that the Islamic faith and social connection helped Somalis cope with the COVID-19 pandemic, as well as other collective traumas.22 Islam also fosters tawakkul (trust in Allah) as a possible means for Muslims to rationalize that the COVID-19 pandemic was a divine decree, and may be a means to preventing mental distress or depression..21
The aim of medicine in Islam is to “preserve health, ward off disease, and restore health when it is lost.”23 There are 28 Quranic verses that focus on the importance of maintaining a healthy lifestyle, and promoting personal hygiene, good diet, nutrition, and alcohol abstinence.24
It is incumbent that Muslim physicians dissuade or prevent their patients from participating in hazardous behaviors that undermine individual and collective well-being.25 While Western cultures emphasize individual choice, individual autonomy is more limited in Islam, as beneficence to others is an act of worship emphasized in the Quran (9:7-8)26 and encouraged by the Prophet (PBUH*) (Muslim 16:1508).27 For example, if a Muslim physician advises an Muslim patient to partake in a healthy behavior that will benefit both the individual and community-at-large, a practicing Muslim would feel obligated and willing to commit such an act for the greater good, rather than possibly disregard the medical advise. According to Amin “worldwide public health organizations are almost in line with the teachings of Islam.”328 Muslims perform daily ablution, wash hands after sleeping, cover one’s face when sneezing, and avoid hand shaking with a leper or infected person.
Tahara (purity or cleanliness) is an essential tenet of the Islamic faith analogous to common practices that prevent, treat, and reduce the chances of contracting or dying from COVID-19. While today’s experts highly recommend social distancing or quarantine to stop and reduce the spread of COVID-19, the Prophet (PBUH) told Muslims to avoid plagued lands 1400 years ago.29 Cleanliness is paramount in Islam. Muslims believe that “cleanliness is half our [Muslims’] faith” (Muslim 223) and “Allah loves cleanliness” (Muslim 2230).27 The Quran also states that Allah loves those who cleanse and purify themselves (2:222).26 Therefore, the acts of cleanliness must precede all Muslims’ behaviors and activities.30
When the Ebola virus reached Nigeria, a Muslim-majority country, the federal government advised citizens to follow the words of the Prophet (PBUH) who urged Muslims to be clean and wash their hands frequently. Rassool30 stressed that cleanliness has significant spiritual (intrinsic) and physical (extrinsic) importance in Islam, similar to Litman et al.’s14 reasonings explained in the Introduction.
The belief and practice of tawakkul helps Muslims to be more resilient during difficult and unpredictable times, such as a pandemic.31 The Muslim worldview on health and illness is unique, with Muslims “receiving illness and death with patience, meditation and prayers.”30 In a Belgian study, it was found that religion played a crucial role in how Muslim women percieved and dealt with illness.32 Health was interpreted to be a trust and blessing from Allah. Participants underlined the importance of accepting illness with gratitude as it is part of Allah’s divine decree. Muslims do so because they consider them natural parts of life and tests from Allah. They see illness as atonement for sins, and death as part of their journey to meet Allah.
According to Hammoudeh et al., most elderly Palestinian women who participated in their study recognized faith and tawakkul as ways of coping, alongside physical activity and healthy eating.33 Muslims are required to work hard towards achieving a well-balanced life (religiously, academically or vocationaly, physically, nutritionally, emotionally, socially, etc.) and to have tawakkul.34
While Muslims rely upon Allah, they must also do their part. When the Prophet (PBUH) was asked by a man whether he should tie his camel and rely upon Allah or leave it loose and rely upon Allah, the answer was, “Tie it and rely (upon Allah)” (at-Tirmidhi 4,11:2517).27 The Quran instructs Muslims “to obey Allah, and obey the Messenger (PBUH), and those in authority among you,” stressing the seeking of credible advice (4:59).26 When a man was injured and two doctors were called to examine him, the Prophet (PBUH) asked who was the better doctor, further indicating the need for superior consultation.35
Various religious practices, such as voluntary prayers, supplications, and Quranic recitations, serve as additional healing aids.32 The Quran mentions deeds that purify Muslims, including generosity (16:90), charity (3:42), compassion (17:23), obligatory prayers (9:103), and almsgiving. Muslims perform these deeds as testaments to their trust in Allah.26 In terms of health and disease, Muslims believe that there is a remedy for every illness or disease on earth, except old age (Sahih al-Bukhari 5678).27 As long as Muslims trust in Allah, their belief of acceptance leads to greater happiness as it includes contentment and peacefulness.
Despite most (40/49, 82%) Muslim-majority countries being LMIC and 100% considered unfree, they had significantly less number of daily new cases than the 116 non-Muslim countries from May 1, 2020 to July 1, 2021. While many Muslim-majority countries were not able to strictly follow social distancing, lockdown, testing, contact tracing, and PPE guidelines, when compared to non-Muslim countries during the 3 global COVID-19 peak dates, they had lower number of COVID-19 cases and deaths per million with statistical significance.
This study shows that Muslims’ practice of tahara is similar to many COVID-19 containment measures, while tawakkul helps Muslims remain resilient and hopeful during difficult unpredictable times, such as living through a pandemic. Strong educational campaigns centered around religious faith that emphasized the practice of strict personal hygiene have proven beneficial for Muslims during this COVID-19 pandemic. It can be beneficial for other countries to stress religious faith and cleanliness practices as a means of attaining greater overall health. It is hoped that this paper brings awareness to the positive practices of the Islamic faith as it relates to COVID-19, and to population and individual health in general.
Research should be conducted in Muslim-majority countries and Muslims living in non-Muslim countries to further study the association of health and adhering to Islamic practices, principles, and beliefs. For example, a number of Muslim countries are currently studying the medicinal benefits of black cumin seed in relation to COVID-19, because the Prophet said that it “can heal all diseases except death” (Sahih al-Bukhari 5687).27 It is hoped that more studies are undertaken to study Islam and Health in general.
*PBUH = Peace Be Upon Him (Prophet Muhammad)
The authors would like to thank Sheilamae Ablay, PhD for her data consultations, Winnie Lu for her data analysis assistance, Samiha Ahmed for her technical editing assistance and insightful critiques, Dr. Tamseela M. Hussain for her medical consultation, Lisa Kahler for her thoughtful feedback, and Maryam O. Funmilayo, MA for her edits. The lead author would like to acknowledge SS for her astuteness; their discussions led to the hypotheses of this research project.
PPM contributed to the concept, design, data acquisition, analysis and results of the research; conducted the literature review, drafted the manuscript and approved final revisions. GG contributed to the design of the research, devised the methodology of and conducted the analysis of the data, created the tables, helped draft the methods and results, and approved final revisions. ZMS contributed to the literature review and offered critical analysis; helped draft the manuscript, provided technical editing, fact-checking and proofreading assistance; and approved final revisions. DMS contributed to the literature review and analysis, helped draft the manuscript, and approved final revisions.
The views expressed in the submitted article are those of the authors and not an official position of our institutions.
Ponn P. Mahayosnand, MPH is a Research Scholar at Ronin Institute. Her research focuses on (1) public health and preventive lifestyle medicine + primary care reform in LMIC, (2) Islam and Health, Prophetic medicine, and health in Gaza, Palestine, and (3) e-mentoring and remote research for women. Ponn earned her BS in Biology, minor in Environmental Health, and concentration in Health Policy and Management from Providence College, and MPH from the University of Connecticut.
Gloria Gheno, MA, MS, PhD is a Research Scholar at Ronin Institute. A data analyst and statistical researcher. Gloria earned her masters in Economics and her professional masters in Economics and Finance from Ca’ Foscari University of Venice, her masters and PhD in Statistics from University of Padova.
ZM Sabra is a medical student at the Islamic University of Gaza. Her research interests are in public health preventive medicine, nutrition & lifestyle medicine and digital health.
DM Sabra is a medical student at the Islamic University of Gaza. In preparation for a speciality in pediatrics, her research interests are in childhood preventive care and nutrition
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.