Ogbeide S. Applying flexibility to the primary care behavioral health model with transient populations. Harvard Public Health Review. Fall 2018;20.
DOI:10.54111/0001/T2
Each year, approximately 3.5 million individuals in the United States experience homelessness (“Hunger and Homelessness,” n.d.). Patients experiencing homelessness have negative health outcomes in part due to decreased access to health care (Fitzpatrick et al., 2011). Additionally, the rate of behavioral health disorders (i.e., mental health and substance use disorders) in patients experiencing homelessness is about 66% (“HCH,” 2006; “National Coalition,” 2014). Follow-up rates for behavioral health services embedded within primary care are higher for transient patient populations when compared to specialty mental health services offered off-site: 16% no-show rate in primary care compared to a 35% no-show rate in specialty mental health settings (Reynolds, Chesney, & Capobianco, 2006). This suggests the need for improved primary care behavioral health integration efforts with this population (Miller et al., 2014; Reynolds et al., 2006). Behavioral health providers have varying roles on the primary care team (Collins et al., 2010; “HCH,” 2006; Heath et al., 2013; Miller-Matero et al., 2014; Robinson & Strosahl, 2009) but the Primary Care Behavioral Health (PCBH) consultation role has not been described with this special population as well as quality improvement efforts with practice change.
Healthcare for the Homeless – Houston (HHH) is a federally qualified health center with three locations in Houston, Texas. The clinics provide medical, behavioral health, dental, and social services to patients experiencing homelessness regardless of their ability to pay. Services at HHH are offered seven days per week. In 2013, there were 9,343 unique patients and 21,765 patient visits. Characteristics of the patient population are found in Table 1. This clinic implemented the PCBH consultation model (Robinson & Reiter, 2016) in 2014 during the inaugural year of behavioral health integration into primary care. The PCBH model is a population-based approach to health care delivery within the primary care setting. A tenet of this model is embedding a “Behavioral Health Consultant” (BHC) into primary care to provide same-day access to patients seeking assistance for the management of behavioral health conditions (e.g., depression, anxiety, Type II Diabetes, high blood pressure, chronic pain). A goal of the PCBH model is to improve and promote overall health and wellness within the primary care population of the clinic.
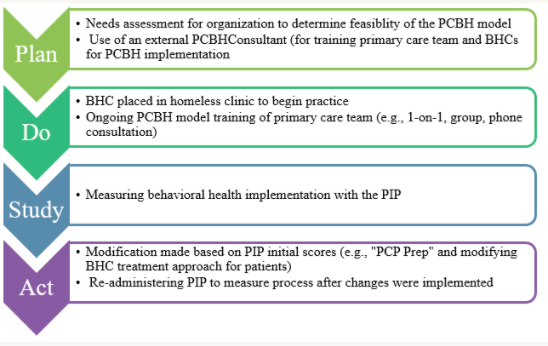
A needs assessment used the Plan-Do-Study-Act (PDSA) approach to determine the logistics of how behavioral health and primary care integration (van Eeghen et al., 2016).The PDSA process for PCBH implementation for HHH is presented in Figure 1. We determined successful implementation would include identifying workspace and clinicians with the skills to thrive in a fast-paced setting with a challenging patient population. We sought clinicians who demonstrated flexibility, confidence, the ability to work effectively on a team, with an understanding of the local patient population, generalist training, the primary care setting knowledge of the PCBH consultation model, and knowledge of brief, behaviorally-focused interventions (Collins et al., 2010; Robinson & Strosahl, 2009).
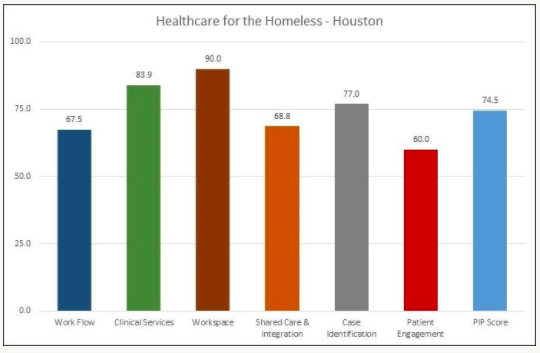
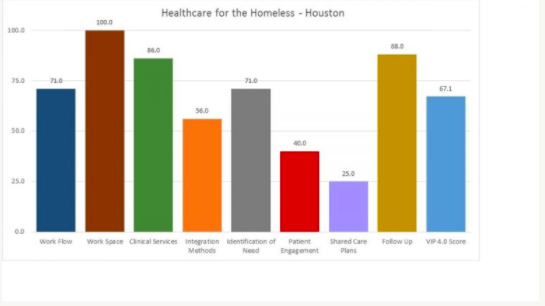
The Practice Integration Profile (PIP), validated measure of integration designed for both quality improvement and research applications (Kessler et al., 2015), was administered to the lead behavioral health consultant, medical director, and executive director in November 2014 – four months after PCBH implementation and again in April 2015 to measure the behavioral health integration progress. Figures 2 and 3 display the PIP data during these two time points in the inaugural year of implementation. We generated an initial median total score of 57.5 (scores range from 0 to 100 with higher scores indicating higher levels of behavioral health integration in primary care settings). Based on that data our team implemented the following changes:
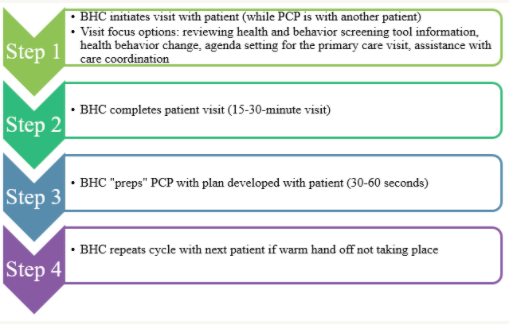
We decided to implement the “PCP preparation” or “PCP prep” which can be described as the BHC consulting with a patient “cold” without a referral question from the PCP (Robinson & Reiter, 2016; Figure 4). In this workflow, the BHC would approach the patient waiting to see a provider and present the role of the BHC. Since there is no referral question, the BHC can start with any of the following example topics: reviewing health and behavior screening tool information, addressing health behavior change, assisting the patient with agenda setting for their primary care visit, or assistance with care coordination. Once the consult is complete, the BHC then provides the PCP with a summary of the consult to “prep” the PCP for the visit. Baker, Bauman, and Beachy (2014) found PCPs viewed the use of PCP prep as positive in practice and encourage continued use an integrated primary care setting
We subsequently administered the PIP 16 weeks after initial administration. Retest generated a total score of 67.1. There was a 20% change in pre/post scores with the PIP. There were additional score changes with the PIP in the domains of identification of need, patient engagement, and follow-up – the areas where we had initiated changes.
There is literature that documents the effectiveness of the PCBH model and the use of BHCs in primary care settings with adults, children, and special populations such as veterans and military service personnel (Bryan, Morrow, & Kanzler, 2009; Bryan et al., 2012; Miller-Matero et al., 2014). More studies are needed to document the clinical effectiveness (e.g., Quadruple Aim: clinical outcomes, patient and provider satisfaction, cost-effectiveness) of the PCBH model with homeless and transient patient populations. Overall, it seems that the PCBH model for transient populations can be an important resource to patients to receive “on-demand” behavioral health services in a setting that is most comfortable to them.
Table 1
Patient Demographics | Percentage (%) |
Gender | |
Female | 39 |
Male | 61 |
Race/Ethnicity | |
African-American/Black | 59 |
Asian/Pacific Islander | 1 |
Caucasian/White | 33 |
Hispanic | 5 |
Other Multiracial/Unreported/Unknown | 2 |
Age (years) | |
< 15 | 1.1 |
15-19 | 0.4 |
20-24 | 5.0 |
25-29 | 10.0 |
30-34 | 10.4 |
35-39 | 10.3 |
40-44 | 13.3 |
45-49 | 16.2 |
50-54 | 17.3 |
55-59 | 10.2 |
60+ | 5.9 |
Note: This is the most recent data from 2013.
Baker, M., Bauman, D., & Beachy, B. (2014, October). Stress, psychological flexibility, and behavioral health satisfaction: An assessment and intervention study with primary care providers. Paper presented at the annual meeting of the Collaborative Family Healthcare Association, Washington, DC.
Bryan, C. J., Corso, M. L., Corso, K. A., Morrow, C. E., Kanzler, K. E., & Ray-Sannerud, B. (2012). Severity of mental health impairment and trajectories of improvement in an integrated primary care clinic. Journal of Consulting and Clinical Psychology, 80(3), 396-403. doi: 10.1037/a0027726
Bryan, C. J., Morrow, C., & Kanzler, K. (2009). Impact of behavioral health consultant interventions on patient symptoms and functioning in an integrated family medicine clinic. Journal of Clinical Psychology, 65(3), 281-293. doi: 10.1002/jclp.20539
Collins, C., Hewson, D. L., Munger, R., & Wade, T. (2010). Evolving models of behavioral health integration in primary care. Publication developed by the Milbank Memorial Fund. ISBN: 978-1-887748-73-5
Gibson, R. L., Mitchell, M. H., & Basile S. K. (1993). Counseling in the elementary school: A comprehensive approach. Boston: Allyn and Bacon.
Fitzpatrick-Lewis, D., Ganann, R., Krishnaratne, S., Ciliska, D., Kouyoumdjian, F., & Hwang, S. W. (2011). Effectiveness of interventions to improve the health and housing status of homeless people: A rapid systematic review. BMC Public Health, 11(638), 1-14. http://www.biomedcentral.com/1471-2458/11/638
HCH Clinician’s Network. (2006, May). Integrating primary & behavioral health care for Homeless people. Healing Hands, 10(2), 1-6.
Heath B., Wise Romero P., & Reynolds K. (2013, March). A standard framework for levels of integrated healthcare. Washington, DC: SAMHSA-HRSA. Center for Integrated Health Solutions.
Kessler, R. S. (2015). Evaluating the process of mental health and primary care: The Practice Integration Profile. Family Medicine and Community Health ,3(1), 63-35. doi: 10.15212/FMCH.2015.0112
Maslow, A. H. (1970). Motivation and personality (2nd ed.). New York: Harper and Row.
Miller-Matero, L. R., Dubaybo, F., Ziadni, M. S., Feit, R., Kvamme, R., Eshelman, A., & … Keimig, W. (2014). Embedding a psychologist into primary care increases access to behavioral health services. Journal of Primary Care & Community Health, 1-5. doi: 10.1177/215013191455083110.1177/2150131914550831
Miller, B. F., Brown Levey, S. M., Payne-Murphy, J. C., & Kwan, B. M. (2014). Outlining the Scope of behavioral health practice in integrated primary care: Dispelling the myth of the one-trick mental health pony. Families, Systems, & Health. Advance online publication. http://dx.doi.org/10.1037/fsh0000070
National Coalition for the Homeless (2014). “Homelessness in America.” Retrieved from http://nationalhomeless.org/about-homelessness/
Ray-Sannerud, B. N., Dolan, D. C., Morrow, C. E., Corso, K. A., Kanzler, K. E., Corso, M. L., … & Bryan, C. J. (2012). Longitudinal outcomes after brief behavioral intervention in an integrated primary care clinic. Families, Systems, & Health, 30(1), 60-71. doi: 10.1037/a0027029
Reust, C. E., Thomlinson, R. P., & Lattie, D. (1999). Keeping or missing the initial behavioral health appointment: A qualitative study of referrals in a primary care setting. Families, Systems, & Health, 17(4), 399-411.
Reynolds, K., Chesney, B., & Capobianco, J. (2006). A collaborative model for integrated mental and physical health care for the individual who is Seriously and Persistently Mentally Ill: The Washtenaw Community Health Organization. Families, Systems, & Health, 24 (1), 19-27. doi: 10.1037/1091-7527.24.1.19
Robinson, P. J., & Reiter, J. T. (2016). Behavioral Consultation and Pprimary care: A guide to integrating services (2nd ed.). New York: Springer.
Robinson, P., & Strosahl, K. (2009). Behavioral health consultation and primary care: Lessons learned. Journal of Clinical Psychology in Medical Settings, 16, 58-71. doi: 10.1007/s10880-009-9145-z
van Eeghen, C., Littenberg, B., Holman, M. D., & Kessler, R. (2016). Integrating behavioral health in primary care using lean workflow analysis: A case study. Journal of the American Board of Family Medicine, 29(3), 385–393. http://doi.org/10.3122/jabfm.2016.03.150186
Stacy Ogbeide, PsyD, MS, ABPP is a primary care behavioral health consultant, board-certified clinical health psychologist, and an assistant professor with the Family Medicine Residency at UT Health San Antonio. She has a cross-appointment in the Department of Psychiatry – Division of Behavioral Medicine at UT Health San Antonio and supervises psychology residents in primary care. Dr. Ogbeide also serves as a consultant for the Greater Houston Behavioral Health Affordable Care Act Initiative, which focuses on engaging and increasing the delivery of integrated health services in Greater Houston and throughout the state of Texas, and recently co-chaired the Primary Care Behavioral Health Special Interest Group and the 2017 Collaborative Family Healthcare Association’s Annual Conference. Dr. Ogbeide has published in the area of integrated care, has conducted more than 80 conference presentations, and teaches graduate courses in behavioral medicine and integrated primary care behavioral health at Our Lady of the Lake University (San Antonio, Texas) and the University of Texas San Antonio.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.