Al-Ghazawi Z, Huang H, Abdulfattah S, Anand A, Adnan Khan M, Mukhtar S. Diagnostic imaging and treatment for sclerosing cholangitis in critically-ill post-COVID-19 patients: a literature review. HPHR. 2022;67.
Review current diagnostic and treatment modalities in post-COVID-19 cholangiopathy to improve screening and risk management
Lin T, Qu K, Xu X, et al. Sclerosing cholangitis in critically ill patients: an important and easily ignored problem based on a German experience. Front Med. 2014;8(1):118-126. doi:10.1007/s11684-014-0306-6
–(“COVID-19” OR “2019 novel coronavirus” OR “2019-nCoV” OR “SARS-CoV-2″) AND
–(“cholangitis” OR “secondary sclerosing cholangitis” OR “cholangiopathy”)
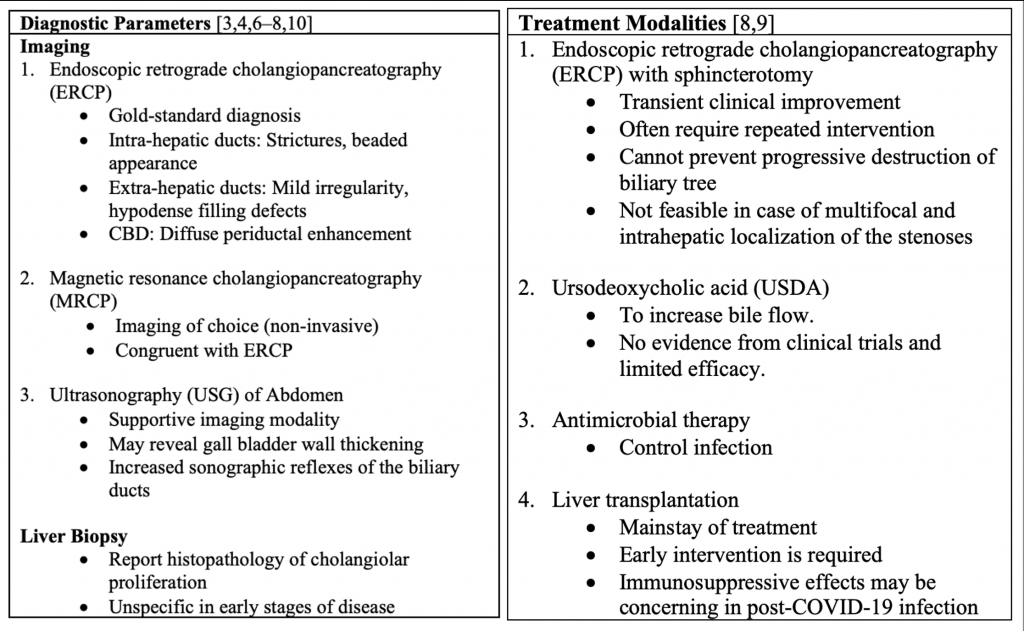
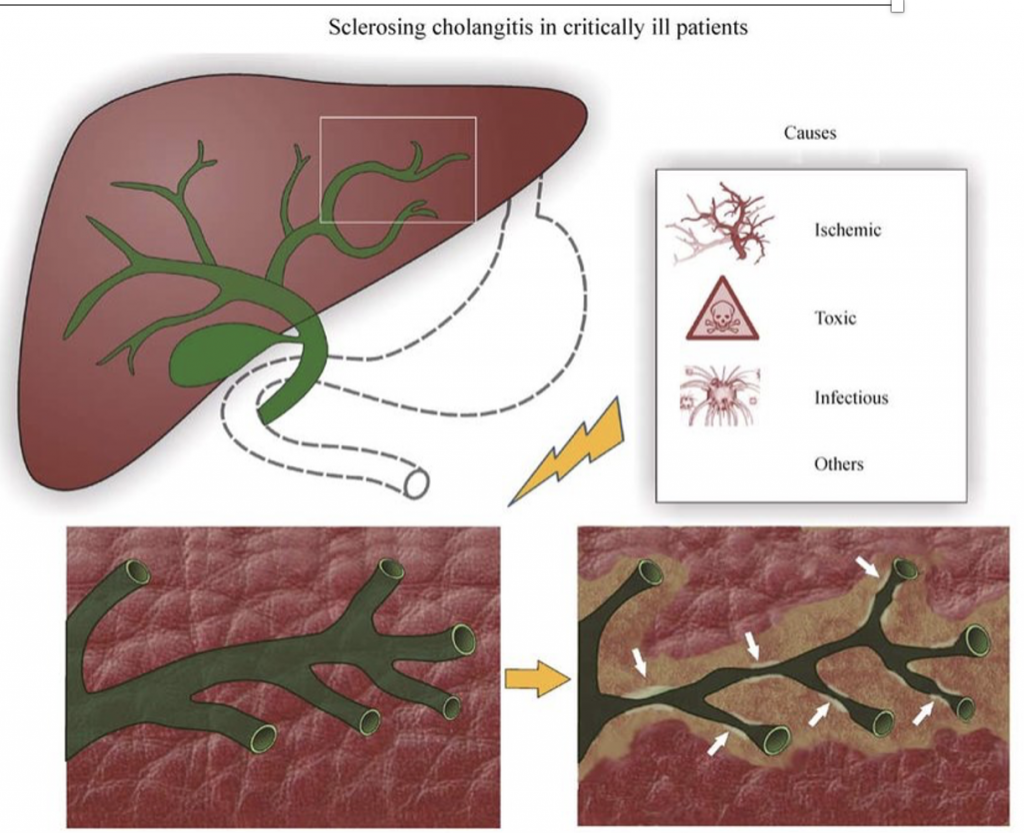
➢Longer-term consequences after SARS-CoV-2 infection are becoming an important burden to societies and healthcare systems
➢Post-COVID-19 cholangiopathy decreases the quality of life for patients
➢Post-COVID-19 sclerosing cholangitis is underrepresented and if missed, could progress to fatal cirrhotic complications
➢Increased awareness and timely diagnosis via imaging is crucial to improve the outcomes of post-COVID-19 cholangiopathy and must be available
➢Liver transplantation are the most effective treatment but concerns regarding health inequity and inaccessibility must be addressed
➢Socioeconomic factors can impact organ transplant accessibility in low-resource settings
➢Treatment options must be further explored to provide better outcomes for the general population and prevent the progression of cirrhosis
➢Future studies should look at the outcome and prognosis of patients receiving liver transplants to better quantify risks and quality of life
We would like to thank Larkin Hospital Team 11 Research Group for this opportunity to present at the Boston Congress of Public Health
1.Edwards K, Allison M, Ghuman S. Secondary sclerosing cholangitis in critically ill patients: a rare disease precipitated by severe SARS-CoV-2 infection. BMJ Case Rep. 2020;13: 237984. doi:10.1136/BCR-2020-237984
2.Roth NC, Kim A, Vitkovski T, Xia J, Ramirez G, Bernstein D, et al. Post-COVID-19 Cholangiopathy: A Novel Entity. Am J Gastroenterol. 2021;116: 1077–1082. doi:10.14309/AJG.0000000000001154
3.Martins P, Verdelho Machado M. Secondary Sclerosing Cholangitis in Critically Ill Patients: An Underdiagnosed Entity. GE – Portuguese Journal of Gastroenterology. 2019;27(2):103-114.
4.Faruqui S, Okoli FC, Olsen SK, Feldman DM, Kalia HS, Park JS, et al. Cholangiopathy After Severe COVID-19: Clinical Features and Prognostic Implications. Am J Gastroenterol. 2021;116: 1414–1425. doi:10.14309/AJG.0000000000001264
5.Durazo FA, Nicholas AA, Mahaffey JJ, Sova S, Evans JJ, Trivella JP, et al. Post-Covid-19 Cholangiopathy-A New Indication for Liver Transplantation: A Case Report. Transplant Proc. 2021;53: 1132–1137. doi:10.1016/J.TRANSPROCEED.2021.03.007
6.Gossard AA, Angulo P, Lindor KD. Secondary sclerosing cholangitis: a comparison to primary sclerosing cholangitis. Am J Gastroenterol. 2005;100: 1330–1333. doi:10.1111/J.1572-0241.2005.41526.X
7.Lee A, Wein AN, Doyle MBM, Chapman WC. Liver transplantation for post-COVID-19 sclerosing cholangitis. BMJ Case Rep. 2021;14. doi:10.1136/BCR-2021-244168
8.Ruemmele P, Hofstaedter F, Gelbmann CM. Secondary sclerosing cholangitis. Nat Rev Gastroenterol Hepatol. 2009;6: 287–295. doi:10.1038/NRGASTRO.2009.46
9.Gelbmann CM, Rümmele P, Wimmer M, Hofstädter F, Göhlmann B, Endlicher E, et al. Ischemic-like cholangiopathy with secondary sclerosing cholangitis in critically ill patients. Am J Gastroenterol. 2007;102: 1221–1229. doi:10.1111/J.1572-0241.2007.01118.X
10.Klindt C, Jensen BE, Brandenburger T, Feldt T, Killer A, Schimmöller L, et al. Secondary sclerosing cholangitis as a complication of severe COVID-19: A case report and review of the literature. Clin case reports. 2021;9. doi:10.1002/CCR3.4068
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.