Knack R, Hanada T, Mayr K, Knack R, Dana S. The importance of telemedicine in Brazil during the Covid-19 outbreak. HPHR. 2021;48. 10.54111/0001/VV11
With the spread of the coronavirus pandemic (COVID -19), the impact on society is increasing, leading to new demands in terms of face-to-face activities, such as work, school, study, physical activities, and even medical appointments, the latter of which have been present in major debates due to the hesitation mediated by the need to go to a medical appointment, but often by the uncertainty of leaving the house and contracting the virus. Given this condition, telemedicine has become a viable and practical option to conduct medical consultations virtually, where communication between doctor and patient can take place via computers with webcams or smartphones, without the need for a face-to-face visit first. The present paper, through literature and documentary research, addresses the results of the use of telemedicine in Brazil adopted by health systems in order to try to avoid physical overcrowding in emergency care settings, while avoiding the risk of transmission to other patients not infected by SARS-CoV2.
Facing the pandemic situation caused by the new coronavirus COVID-19 in the early 2020s, adaptations were necessary to relieve medical services and avoid direct contact between providers and patients in non-emergency conditions.1 In Brazil, one of the strategies imposed was the advent of telemedicine by the single health system. This is not a new technology, other countries already use telemedicine outside of emergency situations, such as the United States, which in 2016 estimated that more than 60% of the country’s hospitals made use of teleconsultations routinely. In the year 2020, with the pandemic, telemedicine was even more used in the U.S., directing greater investments in this sector.2 However, in Brazil, this strategy was not widely incorporated into medical regulations until the emergence of the new pandemic in mid-2020, when a new law n 13. 989/2020, responsible for regulating telemedicine in the country, offering new forms of medical care with easy access to the entire population in the emerging context caused by COVID-19.3 The aim of this study is to evaluate the value of the use of telemedicine in Brazil in the context of the COVID-19 pandemic, since the moment provided great development in this sector.
This review follows the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline for quality of publication reporting.4
The inclusion criteria used were:
Exclusion criteria were:
A search was conducted in the Medical Literature Analysis and Retrieval System Online (MEDLINE), via Pubmed; Scientific Electronic Library Online (SCIELO); Latin American Literature in Health Sciences and the Caribbean – LILACS (via Virtual Health Library – BVS) databases; on August 23, 2021. No date or language limit was applied, the descriptors used are listed in Table 1.
Table1. Mesh terms of search
#1 “Telemedicine”[Mesh] OR (Mobile Health) OR (Health, Mobile) OR (mHealth) OR (Telehealth) OR (eHealth)
#2 “COVID-19″[Mesh]OR (COVID 19) OR (COVID-19 Virus Disease) OR (COVID 19 Virus Disease) OR (COVID-19 Virus Diseases) OR (Disease, COVID-19 Virus) OR (Virus Disease, COVID-19) OR (COVID-19 Virus Infection) OR (COVID 19 Virus Infection) OR (COVID-19 Virus Infections) OR (Infection, COVID-19 Virus) OR (Virus Infection, COVID-19) OR (2019-nCoV Infection) OR (2019 nCoV Infection) OR (2019-nCoV Infections) OR (Infection, 2019-nCoV) OR (Coronavirus Disease-19) OR (Coronavirus Disease 19) OR (2019 Novel Coronavirus Disease) OR (2019 Novel Coronavirus Infection) OR (2019-nCoV Disease) OR (2019 nCoV Disease) OR (2019-nCoV Diseases) OR (Disease, 2019-nCoV) OR COVID19 OR (Coronavirus Disease 2019) OR (Disease 2019, Coronavirus) OR (SARS Coronavirus 2 Infection) OR (SARS-CoV-2 Infection) OR (Infection, SARS-CoV-2) OR (SARS CoV 2 Infection) OR (SARS-CoV-2 Infections) OR (COVID-19 Pandemic) OR (COVID 19 Pandemic) OR (COVID-19 Pandemics) OR (Pandemic, COVID-19)
#3″Brazil”[Mesh] |
Two authors independently screened the articles by reading titles and abstracts through the Rayyan platform,5 a third author evaluated the divergences in inclusion. Eligible references were further analyzed by reading the full text. After the analysis, two authors independently extracted the data. The methodological quality of the studies was also assessed.
The data were extracted from the articles in order to compare them and were summarized in a table (Table 2).
A total of 83 studies were found, among them, 7 were duplicates. Thirteen articles were selected and 7 articles were included after reading the full text.
Table 2.Characteristics of the studies
Author/Year | Description of the use of telemedicine | Conclusions |
Pessalacia,20206 | The advance of the disease has stimulated the interest of governments and health professionals in Information and Communication Technologies. The Telehealth model in Brazil is based on the connection between universities and Primary Health Care, through telecommunication and teleassistance, performing consultation, diagnosis, monitoring, among others. | Training is needed for all health care workers so that the implementation of technology is efficient, as visualized in the pandemic of COVID-19. |
Cerqueira-Silva, 20217 | A communication interface (Telecoronavirus) was created between medical students, institutions and hospitals in 417 municipalities in the state of Bahia, Brazil. | A benefit of telemedicine in the region was elucidated by the possibility of performing high quality telemetry, early detection of the disease, as well as being a simple, low cost strategy with the possibility of performing the consultation at a distance, saving the patient’s displacement and the risk of transmitting the disease to other people. |
Carvalho,20208 | A telemedicine system was implemented to provide remote support for the network of respiratory ICUs, implemented in the state of São Paulo. | The authors pointed out that the use of telemedicine facilitated the training and supervision of the teams and fulfilled the project’s objective, which was to improve the quality of care provided to patients using the single health system. |
Donida, 20209 | The study reported on digital health strategies that were applied in Brazil during the pandemic by COVID-19. Among the strategies used by the Unified Health System, the use of telemedicine for patient care was elucidated. | It was reported that the use of telemedicine favored the pre-clinical care pathways and became essential to avoid overloading health care units. In addition, it was beneficial for sharing exchanges of experiences between medical teams from large centers and small hospitals. |
Harzehein, 202110 | The strategies offered by the Brazilian Unified Health System to strengthen the fight against COVID-19 were described. Among them, TeleSUS was presented as a Telemedicine system created to track, diagnose, treat, and monitor patients with both COVID-19 and Gripal Syndrome. | The use of telemedicine to expand access to primary health care for all Brazilians has been found to be an excellent strategy applied, making it possible to monitor and protect against COVID-19 for 95% of the population covered with a mobile cellular network |
Silva, 202011 | The study aimed to analyze the impact of the use of telemedicine adopted by TelehealthRS-UFRGS, from April to July 2020, to support the health services of the Brazilian Unified Health System. | It was observed that, with the emergence of the pandemic by Covid-19, the use of telemedicine showed a significant and high demand compared to the same period in 2019, most of which was due to questions related to Covid-19. The program offered informational materials about the disease in addition to adequate training for teleconsultation services, which was essential to reach a large number of patients served by the program. |
Caetano, 202012 | A review was conducted to assess the contribution of telehealth to addressing COVID-19 and the strategies used in the country to improve the Unified Health System. | It was inferred that telehealth was essential to increase the ability to combat coronavirus and, keep health services functioning and safer by performing remote screening and treatment assisting in the detection and prevention of COVID-19-related health care. Also emphasizing that the use of this strategy could positively imply public and governmental acceptance for other areas of healthcare in the future, including chronic disease monitoring in Brazil. |
Figure 1. Description of Covid-19 mortality in Brazilian capitals associated with poverty-related indicators, according to the population living on less than US$ 5.5 per day (the range that defines the poverty line, according to the World Bank).
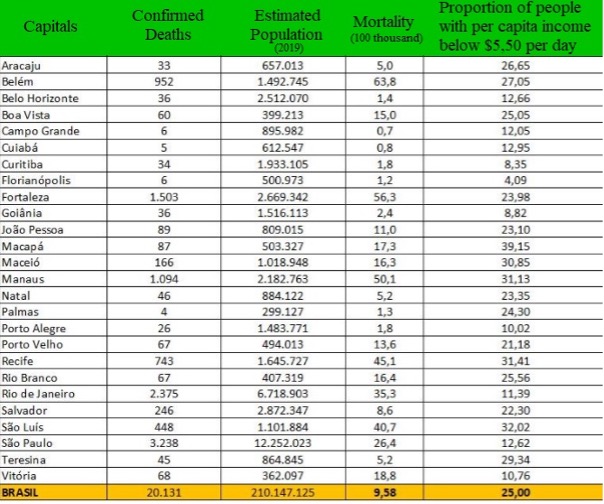
Source: Ministério da Saúde / IBGE (PNAD-C, 2018)13
Figure 2. Proportion of COVID-19 deaths by age group in each group Race/Colour14
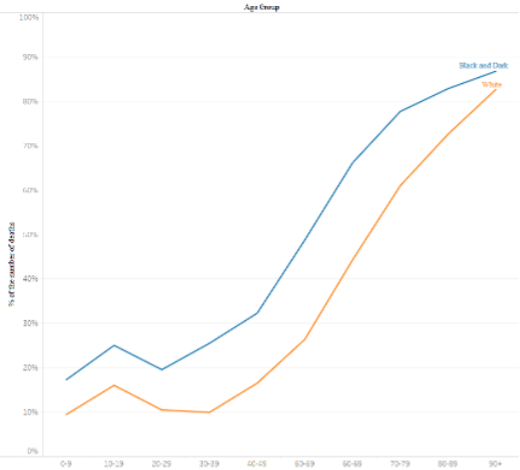
Source: Scientific Technical Center of PUC-Rio (CTC/PUC-Rio)/ Center for Operations and Health Intelligence (2020).
The analyzed articles show positive results to the use of telemedicine in the period of the COVID-19 pandemic, in the training of teams to discuss cases and interdisciplinary consultations, promoting greater access to primary care for several Brazilians; using the single health system (SUS). The studies suggested the importance of training health professionals to use the technology, using the pandemic stimulus to include the method in practice.
Telemedicine emerged in Brazil, concomitant in the world, with the advancement of the internet and globalization. With an initial focus on the educational sphere, Brazil has developed digital health platforms, such as the University Network for Telemedicine( RUTE), which completed 15 years this year, an initiative of the Brazilian Ministry of Science and Technology, coordinated by the National Education and Research Network (RNP), which aims to support the improvement of existing telemedicine projects and encourage the emergence of future inter-institutional work.15
On the threshold of the COVID-19 pandemic, in the midst of the crisis that broke out in the country, the use of this resource became essential amidst the social isolation and the difficulty of managing the disease. On April 15, 2020, the law nº 13.989 was sanctioned, which provides for the use of telemedicine during the crisis caused by the coronavirus (SARS-CoV-2) in Brazil, boosting the use of this method for patient care.16 TeleSus was implemented, making available a pre-clinical health care service, which aims to broadly clarify the population about the disease and when to seek in-person care, in the form of application, whatsapp and phone.
The tragedy caused by COVID -19 provides a unique opportunity for the Brazilian health care system to expand access to health care. The public health system in Brazil is underfunded because it does not receive enough resources to serve the entire population. Nearly 70% of Brazilians do not have health insurance and rely almost exclusively on the public health system, which is a well-structured system but is overburdened with limited resources. The ineffective management of the health system in Brazil is a historical problem that became more evident during the crisis COVID -19.17
Data from 2015 show that Brazil spends about 3.1% of GDP on public health, with an average expenditure of US$525 per inhabitant per year. In other countries where there is a public health system like in Brazil, the average investment is US$3,000 per year. This scenario shows that access to health care in developing countries is still very limited and often precarious.18 The great advantage of telemedicine is the low cost of optimizing the use of medical options, since the specialist is available even in the most remote regions and to the population with the lowest income, democratizing access to health care.
Currently, several health plan operators, laboratories, and clinics offer telemedicine. According to research data, at least 1.7 million services were provided after telemedicine was regulated. The telemedicine program at São Paulo Hospital Albert Einstein has provided more than 270,000 consultations since 2012-approximately 100,000 in 2020. In addition, the hospital has expanded its partnership with the Ministry of Health Northern Region to provide remote care to indigenous communities in the district of Iauaretê, in Upper Rio Negro, Amazonas. 19
The pandemic exacerbated a reality that already existed in Brazil: health inequality. Telemedicine, reflecting the health reality, received greater investment and was concentrated in the large cities that have large health centers, the capitals in the southeast and south of the country. The population in the northern and northeastern regions, far from these centers, already suffers from the tragedy of lack of access to primary care and health professionals. On the verge of social isolation and lack of access, often even to information, they are more and more abandoned to their fate.20 These negative effects are clearly reflected in the mortality of the population associated with low income. Figure 1, produced by the Ministry of Health/IBGE (PNAD-C, 2018), shows the relationship between the impact of Covid-19 and the structural causes of inequality in the country according to the proportion of Brazilian capitals and the rates of population living below the poverty line. It can be concluded that capitals with a larger number of people below the poverty line have a higher Covid-19 mortality rate.13
Against the backdrop of “pandemic racism,” the data, the epidemiological bulletins of the Brazilian Ministry of Health, show that black mortality exceeds that of whites (Figure2). The Center for Operations and Health Intelligence (NOIS) analysis examined data on 30,000 cases with discharge or death by May 18, 2020, and indicated that black and brown people accounted for 55% of mortality during this period, while 38% were white. The data shows that the black population suffers the consequences of lack of access to health care, which inevitably means the non-granting of rights that should be equally guaranteed.
In 2019, a healthtech startup, “Afro Saúde”, was created by two Brazilian entrepreneurs who developed the concept of “Telecorona da Periferia”. The proposal is to offer a call center targeting people from the periphery to answer questions and avoid overcrowding Emergency Care Units (UPA). From March to June 2020, the platform helped more than 230 people living in the suburbs, in the complex Northeast Amaralinaas, which together add up these regions of the capital of Bahia to 250 thousand people. The patients used the communication channels to ask questions about isolation with four people living in one room and about the symptoms of COVID -19, among others.21
In Brazil, according to the Brazilian Institute for Geography and Statistics (IBGE) in 2019, it was found that of the 10% of the population with the lowest per capita income in Brazil, 75.2% are black and only 23.7% are white. (SIS IBGE 2020).22 Thus, the black population is found to have a greater negative impact on the lack of access to telemedicine information and technologies for early screening of infections by COVID -19, and this could be a hypothesis that justifies the defense of the higher mortality of the black population by COVID-19.
Due to an adverse scenario during the pandemic, indicating impaired access to care, it is possible that the public health system is overloaded due to high demand, at the expense of this population that did not receive adequate treatment early on. We then hypothesize that the continuity of telemedicine after the pandemic could have a beneficial character by relieving the system of personal care, which could lead to better implementation and follow-up of cases.
Our data from this literature review suggests that the implementation of a multimodal telemedicine system focused on the pandemic of COVID-19 is feasible in the country, not only during the present emergency setting, but also as a strategy to be continued after the stabilization of the pandemic setting, due to the great benefits elucidated by the reports described across the country.
The worldwide value of COVID-19 has created an urgency to make health services available to everyone, anytime, anywhere, and despite the negative impacts of the pandemic on global health, the advances in digital health in developing countries should be seen as a positive value.
After the assault on Gaza in May 2021, the healthcare system and sewage systems, already in poor condition, were further decimated, with destruction affecting the main COVID–19 lab.10,11 With the goal of developing a more sustainable healthcare infrastructure to compensate, the medical reserves were proposed.10 Within this proposal, underemployed healthcare professionals in Gaza will be trained and work in 4 divisions to support Gaza’s healthcare network development. One division is the healthcare education and community outreach team, which will serve to support1 emergency health services and2 long–term preventive primary care services.
Part of the education and outreach plan is to involve elders from Gaza’s various neighborhoods,which would allow the community to be directly involved in its own healthcare support system.10 This community-based approach’s importance was made evident in Afghanistan, where the authors stated there needs to be more focus on building public trust especially in government or larger organizations.7 This critical point would be addressed by the incorporation of these neighborhood elders. By seeking support from local leaders, a more trusting relationship can be ensured. This technique is further supported by Ethiopia’s use of task forces where individuals spread information to community members at the personal level.4 Syria also used a similar framework as a part of their Volunteers Against Corona initiative.9
Once this trust is built between the government, health educators, and its citizens, there is an easy translation of information. Gazans have a high literacy rate, so it will be effective to use social media and other text–based platforms to spread important COVID–19 related messages.10 Utilizing social media, health education messages can more effectively reach a greater population similar to Syria and Lebanon’s successful COVID social media campaigns.10 Lessons learned from Bangladesh and Somalia indicate that both countries may have benefited from technology use.5,6
Rafael Knack is a endocrinologist at Israelita Albert Einstein Hospital, São Paulo, Brazil
Taliê Hanada is a medical student, in the last year of medical school.
Kamilla Mayr is a medical Student at Universidade Metropolitana de Santos, Brazil.
Renata Knack is the director of research at the Israelita Albert Einstein Hospital, São Paulo, Brazil
Samy Dana is an economist with a Ph.D in Financee
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.