Chopra C, Youssef A, Pecora C, Ghisletta L. Bridging the gap in surgical patient education: a visual-based approach. HPHR.
2021; 32.
DOI: 10.54111/0001/FF8
Patient education is an essential aspect of surgical practice, as it improves patient compliance, trust in providers, and health outcomes (Paterick, 2017). Barriers to education, such as language and health literacy, are a challenge to this process (Behmer Hansen, 2020). The Census Bureau’s 2018 American Community Survey found that 38% of English-second-language (ESL) Americans speak English “less than very well” (McHugh, 2019). Despite this, most patient education material is only guaranteed in the English language, and is written at a reading level much higher than the national average (Behmer Hansen, 2020). Beyond issues of informed consent and procedure comprehension, faulty engagement with healthcare providers is a source of great risk to patient health (Sharma, 2018).
Failure to meet the low health literacy requirements of a patient population occurs regardless of surgical specialty. Neurosurgical patient education materials have been labeled as difficult to understand, creating a significant barrier in maintaining patient engagement (Ramos, 2019). Orthopedic and hand surgery education materials have also been found to be at unrealistically high reading levels (Hadden 2016, Prince 2019).
Helping to reduce barriers in access and comprehension, the internet has become a widely-used tool for patients, providing a litany of health education material of varying breadth and depth (Behmer Hansen, 2020). This is supported by the fact that 61% of US adults have used the internet to look up health information (Cohen, 2011). The content of surgical educational material in this realm, however, is still at a higher average reading level than that recommended by the National Institutes of Health (NIH) and American Medical Association (AMA), averaging a 10th-grade reading level rather than the recommended 6th-grade or lower (Behmer Hansen, 2020). Furthermore, the lack of physician review of materials for accuracy and relevance leave much to be desired in this medium. In fact, one study on googling illnesses in children demonstrated that of 500 sites surveyed, only 39% hosted accurate clinical information (Scullard, 2010). This highlights the need for finding alternative measures of accurately communicating information to patients in an easily-accessible manner.
To address issues of comprehension, surgical patient education initiatives thus far have attempted to focus on procedural highlights (Villanueva, 2018). Limitations in this method include failure to capture all the information necessary for the patient, as well as a failure to circumvent the limitations in written content. Other multimedia-based approaches have been adopted for enhanced engagement, but still encounter difficulties addressing education and language barriers (Agarwal, 2020). Given this, illustration provides a promising solution in circumventing literacy and language-based comprehension issues (Park, 2016). Despite this, there exist limitations in current illustration-oriented education materials. First, these materials are still often accompanied by extensive written description that complicates comprehension. Second, these materials are typically privately owned and thus cost-prohibitive to healthcare settings that need them most – those with little or no funding for education material.
Enhancing the quality of surgical education among low health literacy and ESL patients requires a directed approach that addresses the above-mentioned obstacles. Material must be generated for highly prevalent surgical scenarios and made publicly available. To achieve this end, we established a 3-stage process for the development of standardized, visual-based educational material. Each phase of development is described below with burn care education provided as a corresponding example.
The research team’s affiliated county hospital was used as a primary site for development of our tool. Their surgery clinic is high-volume and sees a variety of perioperative patients daily. Physician teams first identified procedures and perioperative care plans based on their prevalence or the complicated nature of the patient education. Once selected, a series of questions on content and description of procedures and plans was established. Questions included “What is the relevant anatomy involved in this procedure/plan?”, and “What are the most common difficulties encountered in explaining this procedure to patients?”.
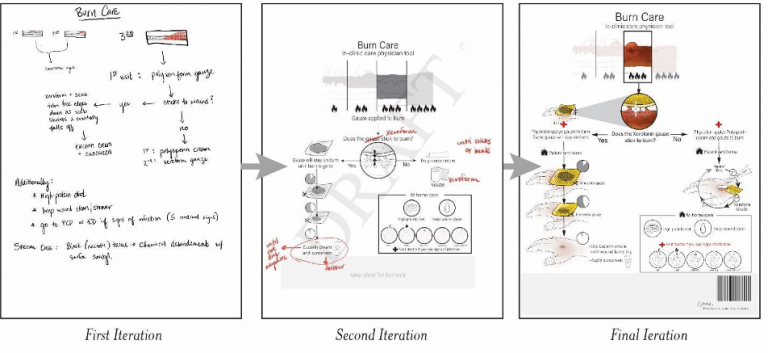
The first iteration of the visual tool was largely composed of verbal information gathered during interviews with clinicians (Figure 1). Attention was paid to areas of explanation that were particularly difficult to convey, and a special note was made of ‘must-have’ information that should be highlighted in the document. Information was generally formatted in a flowchart to allow for ease of instruction and visualization.

The second iteration was made by the medical illustrator and was based on the content of the first iteration (Figure 2). This version sought to convert verbal information into illustration wherever possible, keeping written language down to individual words and small phrases. Images were designed to be as realistic as possible while remaining easy to understand.
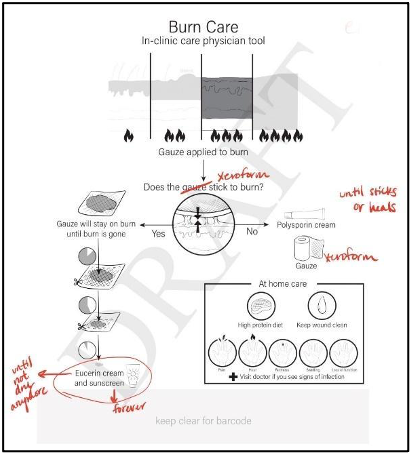
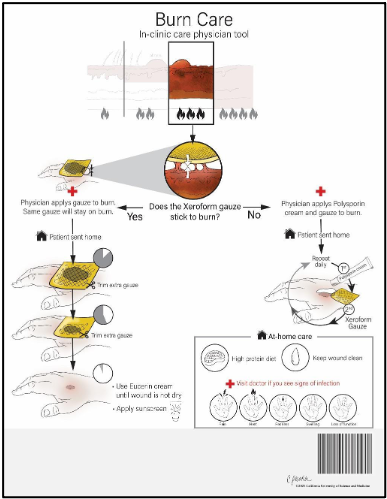
Of note, advanced vocabulary was only included when absolutely necessary. For example, the word ‘xeroform’ gauze was preserved in the burn care document because, despite the general public not generally knowing what xeroform gauze is, conflation of this type of gauze with a dry gauze would be dangerous to the wound healing process. The assumption when including this term in the educational document is that the physician will physically provide the accompanying gauze to the patient. This may be a limitation of the tool depending on whether or not the healthcare institution issuing the document also provides wound care equipment to their patients.
Validation of our educational tool requires use and interpretation on both the clinical and patient side. Clinically, the tool must be 1) easy to access, 2) clinically relevant and up-to-date, and 3) comprehensive and usable as an adjunct to existing educational methods. Furthermore, these tools should be deemed appropriate for use by not only the physician, but the entire treatment team in the clinic (e.g. nurses, medical assistants, medical students), as these individuals are often involved in educating patients and should also have the tool at their disposal. Such validation can be analyzed qualitatively and quantitatively, although an appropriate survey design to achieve this is still in development.
Language and literacy-sensitive educational tools are difficult to develop. Particularly in a surgical setting, it is critical the clinical team is able to convey complex information while ensuring comprehension. The caveats in explaining procedural steps, timelines, and complications is a lot of information to convey in one visit. The use of illustration shows promise in educating a patient population overwhelmed by purely written or verbal instruction. While achieving this goal requires extensive workshopping between the physician, medical illustrator, research team, and patient, it also proves to be a transparent and outcome-driven approach.
To fully evaluate the efficacy of this proposed model of education, our subsequent aims are to standardize patient response to these tools through in-clinic surveys. Target populations would include 1) patients that receive illustration-based education in addition to standard-of-care education, and 2) patients who receive standard-of-care education alone. Quantifying patient perspectives on this tool will allow for further refinement that remains patient-oriented and effective.
Another key aspect we intend to develop is translation to other languages. While illustrations are advantageous in their general ability for universal comprehension, the small words and phrases that are included should be in a patient’s native language to maximize their relevance. Finally, our eventual aim is to make these materials publicly available for use by any interested healthcare institution or provider. Making these materials free of cost, widely available, and adherent to language and content requirements set forth by medical and educational entities will enhance health outcomes for a broad surgical patient population.
Agarwal, N., Funahashi, R., Taylor, T., Jorge, A., Feroze, R., Zhou, J., Hansberry, D. R., Gross, B. A., Jankowitz, B. T., & Friedlander, R. M. (2020). Patient Education and Engagement Through Multimedia: A Prospective Pilot Study on Health Literacy in Patients with Cerebral Aneurysms. World neurosurgery, 138, e819–e826. https://doi.org/10.1016/j.wneu.2020.03.099
Behmer Hansen, R., Gold, J., Lad, M., Gupta, R., Ganapa, S., & Mammis, A. (2020). Health literacy among neurosurgery and other surgical subspecialties: Readability of online patient materials found with Google. Clinical neurology and neurosurgery, 197, 106141. https://doi.org/10.1016/j.clineuro.2020.106141
Cohen RA, Adams PF. Use of the Internet for health information: United States, 2009. NCHS data brief, no 66. Hyattsville, MD: National Center for Health Statistics. 2011.
Hadden, K., Prince, L. Y., Schnaekel, A., Couch, C. G., Stephenson, J. M., & Wyrick, T. O. (2016). Readability of Patient Education Materials in Hand Surgery and Health Literacy Best Practices for Improvement. The Journal of hand surgery, 41(8), 825–832. https://doi.org/10.1016/j.jhsa.2016.05.006
Health literacy month: Health literacy resources. (2020). Retrieved from https://calmedu.libguides.com/c.php?g=878962&p=6315579
Lopez Ramos, C., Williams, J. E., Bababekov, Y. J., Chang, D. C., Carter, B. S., & Jones, P. S. (2019). Assessing the Understandability and Actionability of Online Neurosurgical Patient Education Materials. World neurosurgery, 130, e588–e597. https://doi.org/10.1016/j.wneu.2019.06.166
McHugh, P. (2019, October 29). 67.3 million in the United states spoke a foreign language at home in 2018. https://cis.org/Report/673-Million-United-States-Spoke-Foreign-Language-Home-2018.
Park, J. Zuniga, J. Effectiveness of using picture-based health education for people with low health literacy: An integrative review. Taylor & Francis. https://www.tandfonline.com/doi/full/10.1080/2331205X.2016.1264679.
Paterick, T. E., Patel, N., Tajik, A. J., & Chandrasekaran, K. (2017). Improving health outcomes through patient education and partnerships with patients. Proceedings (Baylor University. Medical Center), 30(1), 112–113. https://doi.org/10.1080/08998280.2017.11929552
Prince, L. Y., Mears, S. C., Watson, J. C., & Hadden, K. B. (2019). Health Literacy Evaluation of Opioid Patient Education Materials for Orthopaedic Surgery. Journal of surgical orthopaedic advances, 28(3), 232–236.
Sharma, A. E., U, S., KL, C., Al., E., RE, D., JH, H., … EJ, S. (2018, November 1). Patient Engagement In Health Care Safety: An Overview Of Mixed-Quality Evidence: Health Affairs Journal. Health Affairs. https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.0716.
Scullard, P., Peacock, C., & Davies, P. (2010). Googling children’s health: reliability of medical advice on the internet. Archives of disease in childhood, 95(8), 580–582. https://doi.org/10.1136/adc.2009.168856
Villanueva, C., Talwar, A., & Doyle, M. (2018). Improving informed consent in cardiac surgery by enhancing preoperative education. Patient education and counseling, 101(12), 2047–2053. https://doi.org/10.1016/j.pec.2018.06.008
Christina is a third-year medical student at the California University of Science & Medicine. She comes from a background in biological anthropology and healthcare project management, and has since developed her interests in surgery and surgical education. In her free time she enjoys writing, baking, and hiking in the Southern California area.
Youssef is a first-year medical student at the California University of Science & Medicine. He has a background in Physiological Sciences and Public Health with a focus in Epidemiology and is exploring the interaction of these fields in surgery and patient education. In his free time, he enjoys martial arts, basketball, and spending time with his family.
Christina is a certified medical illustrator at the California University of Science & Medicine. She comes from a background in anatomy and art and enjoys transforming complex medical topics into comprehendible visuals.
Dr. Leslie Ghisletta, M.D., F.A.C.S. is a trauma, burn and critical care surgeon practicing at Arrowhead Regional Medical Center. She did her residency at Drexel University College of Medicine in Philadelphia and fellowship at Emory University School of Medicine and practiced in her field for five years at Rutgers New Jersey Medical School before moving back home to California. She spends her free time with her rescue Shih Tzu and rescue parrots.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.