Schmid A. Preventing pandemics and containing disease: a proposed symptoms-based syndromic surveillance system. HPHR. 2021; 31.
DOI:10.54111/0001/EE21
Several disease surveillance systems are in place to track rises in disease incidence; however, the current global landscape concerning the spread of COVID-19 has demonstrated our lack of ability to stop the spread of disease efficiently, exposing inadequate local and global pandemic preparedness and placing extreme stress on healthcare facilities and medical supply demands. Current surveillance methods are insufficient. A healthcare provider must see patients before their symptoms are reported, allowing for unchecked transmission of disease. Access to quality healthcare is limited and inconceivable in many parts of the world. Current methods also lack communication and integration. Current approaches do not track disease early enough, leading to delays in outbreak detection and delays in response to these outbreaks. The current systems in place are acceptable for tracking disease but do not allow for effective prevention of disease spread. A symptoms-based surveillance system was designed that addresses current limitations and adequately detects disease. The system improves overall health surveillance with a focus on early detection of both known and unknown diseases, prevents disease transmission within the community, and can be employed globally, thus reducing the potential for future pandemics. The platform is a self-reported, symptoms-based syndromic surveillance system that is universal, interactive, integrated, and combined with artificial intelligence (AI). The platform will identify potential and confirmed outbreaks and advise individuals using AI-based pattern recognition. To determine when further action is warranted by individuals and public health officials, the AI collects, stores, and monitors symptom-based data and alerts in response to spikes in illness. The AI also tracks and predicts potential disease spread. The proposed platform provides an innovative and scalable alternative to the existing fragmented and ineffective health surveillance systems.
Keywords: syndromic surveillance, artificial intelligence, pandemic, proposal, public health, organizational models
Current surveillance methods only track provider-reported symptoms and cases of disease (CDC, 2020; NYTimes, 2020; Johns Hopkins, 2020; nCoV2019, 2020; HealthMap, 2020) presenting a multitude of problems. Patients must be seen by a healthcare provider before their symptoms are reported. Delay of care is a common problem with up to 43% of Americans reporting they were not able to be seen on time for urgent matters (Murray & Berwick, 2003; Strunk & Cunningham, 2002; Greenblatt, 2002). Patients often have already had symptoms, potentially for weeks, before being seen. People hesitant to seek care may travel or have contact with other people while knowingly or unknowingly infected, further transmitting disease.
Another problem with current disease surveillance methods is access to healthcare. Access to quality healthcare is limited in parts of the United States and in parts of the world (Peters et al., 2008). Underserved communities lack access to healthcare, and up to 35% of these individuals report not receiving care at all (CDC, 2018; Frye, 2020; U.S. Department of Health and Human Services (HHS), 2020). People in these rural communities are forced to wait days to weeks before being seen by a healthcare professional, must travel in poor conditions, or do not seek care at all. Geographic accessibility and travel can be limited in developing countries and is required not only for people to seek care and travel to healthcare facilities but also for the distribution of healthcare-related items (drugs, vaccines, etc.) (Peters et al., 2008).
The third problem with current methods is the lack of communication and integration. Existing organizations and their surveillance systems do not communicate with each other, and the data is not integrated into one central location.
Other limitations are systemic and logistical. Rural areas and developing countries have power and electricity limitations, supply-chain limitations, and problems with internet or cellular network access. This limits current surveillance methods in regards to addressing problems out in the field. Rural areas are challenging to reach, and reporting is not done in these areas.
Current methods do not track disease early enough in the disease process to catch symptoms, contain disease hotspots, and prevent future outbreaks and pandemics. These problems lead to delays in outbreak detection and delays in response to these outbreaks. The current systems in place are acceptable for tracking disease but do not allow for effective, proactive prevention of disease spread.
The goal of this proposal is to design a symptoms-based surveillance system that does three things.
The proposed solution is a free, self-reported, symptoms-based syndromic surveillance system that is universal, interactive, integrative, and combined with AI, which utilizes short message service (SMS; text-messaging) and interactive voice response (IVR; calling) to identify and contain hotspots during the early stages of an outbreak. The framework uses self-reported data via personal mobile phones and is available in urban and rural areas worldwide.
Integrated: one centralized system
Artificial intelligence (AI)
Pattern-based recognition system
Interactive: communication between system and user
Disease education, alerts, and warnings
Next-steps and follow-up
Self-reporting: mobile phone SMS/IVR
Rapid deployment, simple
Increased access and global penetration
Collaboration: governments, public health, hospital systems
This platform will identify both potential and confirmed local disease outbreaks and advise individuals to follow appropriate care, thus preventing future epidemics and pandemics.
Small-scale surveillance systems demonstrate proof of concept for the proposal. Zenysis is a mobile-based emergency response and disease surveillance system. It utilized a centralized, integrated server and was used to prevent Cholera in Mozambique. Zenysis was able to recognize hotspots and sources of water contamination, allocate supplies and vaccines, and get the case count from 400 to zero in three weeks (Zenysis, 2020).
The Early Warning, Alert, and Response System (EWARS) through the World Health Organization (WHO) and Global EWARS project improves disease detection and surveillance in emergency settings. It is a mobile phone, field-based reporting and management system deployed in remote and challenging field settings where there is no reliable internet or electricity (WHO, 2020). Out-of-reach populations lacking broadband internet and cellular service are accessible with this platform. Similar to EWARS, the proposed system could be run for weeks, in hundreds of languages, on a local server with mobile phones, laptops, and solar generators.
The Mobile-Based Surveillance Quest Using IT (MOSQUIT) in India is a digital, mobile-phone-based Malaria surveillance system. It offers real-time tracking of disease, identification and management of outbreaks, and runs on a central server. It also allows for data collection from rural and slum areas (Neydenova, 2016). ProMED Mail (PMM) is an open and free to use, global, email-based surveillance system from the International Society for Infectious Disease (Madoff & Woodall, 2005). PMM caught a Cholera outbreak in the Philippines three weeks before the WHO and a Cholera outbreak in Peru eight weeks before the WHO (Madoff & Woodall, 2005). PMM has also been the first system to detect and report on numerous disease outbreaks, including SARS, MERS, Ebola, and Zika (Carrion & Madoff, 2017). Drew et al. (2020) have used this concept in Wales, United Kingdom, to predict geographical hotspots of COVID-19 incidence five to seven days before public health reports. While several countries have previously implemented small-scale, local, mobile-based health surveillance systems, the lack of central integration and global expansion misses early detection of outbreaks, leading to inaccurate reporting and unchecked transmission of disease.
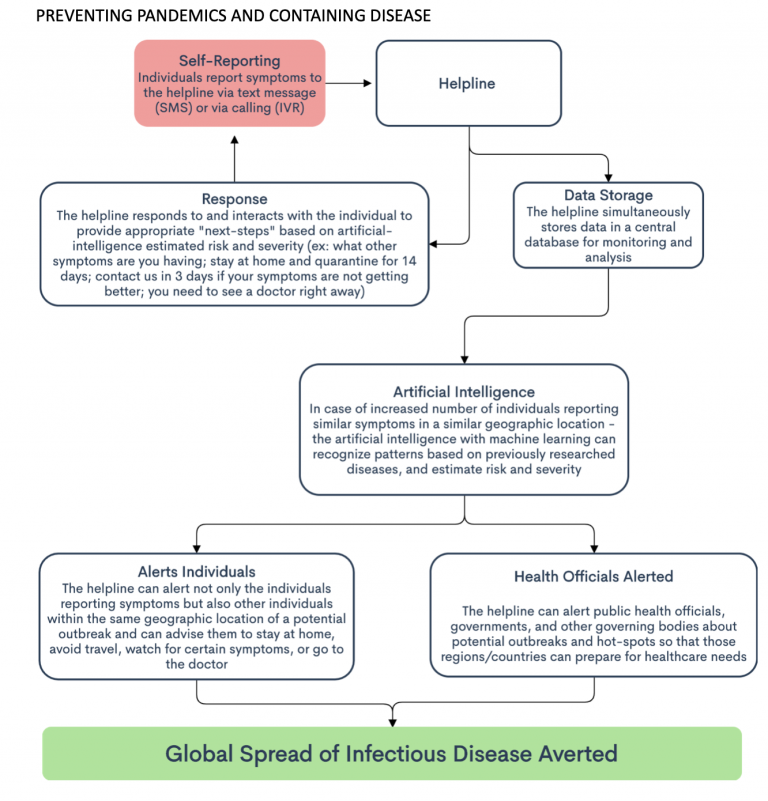
The system begins when individuals text or call into the system to report their symptoms. The symptoms are added to a central database, and various metrics are recorded (i.e., location). Subjective and objective information is tracked and documented while leaving out protected health information (PHI). AI interprets what is texted or called in. The AI can communicate and interact with the individual, gathering potentially useful and pertinent information. AI makes a suggestion to the individual for what to do next. The system estimates severity and urgency based on the individual’s responses and recommends next-steps such as quarantine, wearing a mask, or going straight to see a doctor. The symptoms added to the database are simultaneously analyzed. The AI with machine learning notes trends, similarities, differences, patterns, etc. based on previously researched outbreaks and diseases. These incidences of increased reporting are rated on severity and risk and are flagged for human review. Officials can then retrieve the data, analyze the flagged incidences, and consider the severity and risk rating. Once potential hotspots or areas of potential outbreak are identified, swift action can be taken to alert the public, implement public health regulations and restrictions, and prevent further spread.
Information collected is de-identified and HIPAA compliant. United States federal law allows the sharing of healthcare-related information with those conducting public health surveillance (45 CFR 164.512(b)). International health regulations implemented by the Global Outbreak Alert and Response Network (GOARN) permit the sharing of health information among countries (Mackenzie et al., 2014).
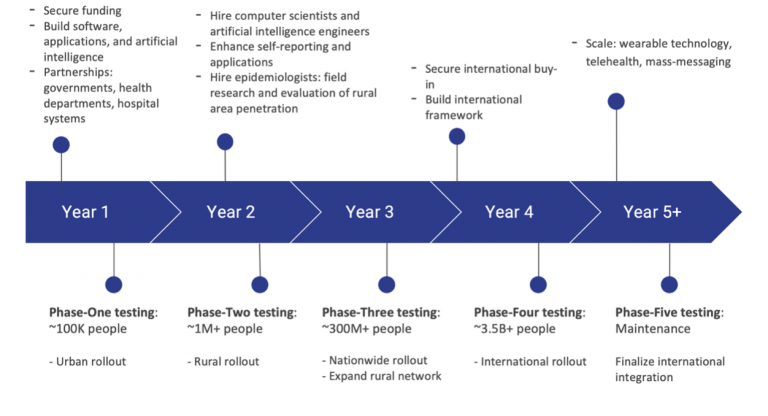
Through solidification of partnerships with biotechnology companies and global legislative bodies, the system can expand and be accessible worldwide. As demonstrated by Drew et al. (2020), mobile-based tools can be rapidly deployed. Combined with AI and machine learning, the system could identify emerging patterns of disease exposure, symptom onset, disease trajectory, and clinical outcomes. Future growth could integrate healthcare services such as wearable devices, robotic telemedicine carts, virtual telemedicine offices, and remote monitoring.
Technology is automated, fast, scalable, and available 24/7. Mobile phones and networks offer acceptable quality at an affordable cost. The AI-based control center decreases the HR burden. Once built, the system can easily be maintained. The system’s proactive approach can strengthen worldwide supply chains and prevent their collapse. Vaccines, personal protective equipment, and necessary healthcare items can be appropriately allocated.
The need to see a healthcare provider before symptoms are reported is averted through mobile-based reporting by individuals, allowing for earlier reporting and earlier action by officials to prevent disease spread. Mobile-based reporting also bypasses the need for smart phones and broadband internet connection. Text messaging is the most used data service in the world, and the number one preferred customer support channel in the United States (Nielsen, 2013; Twilio, 2016). Interactive voice response (IVR) can provide voice-to-text and text-to-voice services and can be used by those individuals unable to text. 94% of the population of advanced economies and 78% of those in emerging economies have mobile phones (Silver, 2019; Pew Research Center, 2019).
To determine when further action is warranted by individuals and public health officials, our AI’s memory and functional ability will allow for collection, storage, and monitoring of symptom-based data. The system tracks potential disease spread and alerts in response to increases in illness.
The global, widespread usage of personal mobile phones, and the previous success of regional mobile-based health surveillance systems, emphasize the feasibility and applicability of this concept. Implementation of AI-based pattern recognition and tracking provides an innovative and scalable alternative to the existing fragmented and mostly ineffective health surveillance systems.
Alampay, E. (2003). Reporting Police Wrongdoing via SMS in the Philippines. eGovernment for Development Information Exchange. Text 2920/117 (2020). beoutbreakprepared/nCoV2019. Beoutbreakprepared, Github. https://github.com/beoutbreakprepared/nCoV2019.
Carrion, M., & Madoff, L. C. (2017). ProMED-mail: 22 years of digital surveillance of emerging infectious diseases. Int Health, 9(3), 177-183. doi:10.1093/inthealth/ihx014
(2020). COVID-19. Novel Coronavirus (COVID-19). HealthMap. https://www.healthmap.org/covid-19/
(2020). COVID-19 United States Cases by County. Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/us-map.
(2020). COVID Worldwide Realtime Symptom Tracker. Retrieved from https://g-covidtracker.firebaseapp.com/tracker
Drew, D. A., Nguyen, L. H., Steves, C. J., Menni, C., Freydin, M., Varsavsky, T., … & Spector, T. D. (2020). Rapid implementation of mobile technology for real-time epidemiology of COVID-19. Science.
(2020). Early Warning, Alert, and Response System (EWARS). World Health Organization. Retrieved from https://www.who.int/emergencies/surveillance/early-warning-alert-and-response-system-ewars
(2020). FAQ: COVID-19 Data and Surveillance. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/faq-surveillance.html.
Frye, I. (2020). The Impact of Underserved Communities in Times of Crisis. Healthcare Information and Management Systems Society. Retrieved from https://www.himss.org/resources/impact-underserved-communities-times-crisis
(2020). Global EWARS Project. World Health Organization. Retrieved from http://ewars-project.org/
(2016). Global Mobile Messaging Consumer Report 2016. Twilio. Retrieved from
https://www.twilio.com/learn/commerce-communications/how-consumers-use-messaging
Greenblatt, J. (2002). Access to Urgent Medical Care, 2001. Rockville, Md: Agency for Healthcare Research and Quality, Statistical brief number 08. Retrieved from https://meps.ahrq.gov/data_files/publications/st8/stat08.shtml
Kshetri, N. (2014). Global entrepreneurship: environment and strategy. Routledge.
Mackenzie, J. S., Drury, P., Arthur, R. R., Ryan, M. J., Grein, T., Slattery, R., . . . Bejtullahu, A. (2014). The global outbreak alert and response network. Glob Public Health, 9(9), 1023-1039. doi:10.1080/17441692.2014.951870
Madoff, L. C., & Woodall, J. P. (2005). The internet and the global monitoring of emerging diseases: lessons from the first 10 years of ProMED-mail. Arch Med Res, 36(6), 724-730. doi:10.1016/j.arcmed.2005.06.005
(2019). Mobile Fact Sheet. Pew Research Center. Retrieved from https://www.pewresearch.org/internet/fact-sheet/mobile/
Murray, M., & Berwick, D. M. (2003). Advanced access: reducing waiting and delays in primary care. JAMA, 289(8), 1035-1040. doi:10.1001/jama.289.8.1035
Naydenova, E. (2016). Mobile-based Surveillance Quest using IT (MoSQuIT), India. Social Innovation in Health Initiative Case Collection. [Online] WHO, Geneva: Social Innovation in Health Initiative, Available at: https://www.socialinnovationinhealth.org/downloads/Case_Studies/MoSQuIT_SIHI_Case_Collection.pdf
(2020). nytimes/covid-19-data. New York Times, Github. https://github.com/nytimes/covid-19-data.
Peters, D. H., Garg, A., Bloom, G., Walker, D. G., Brieger, W. R., & Rahman, M. H. (2008). Poverty and access to health care in developing countries. Ann N Y Acad Sci, 1136, 161-171. doi:10.1196/annals.1425.011
Silver, L. (2019). Smartphone Ownership Is Growing Rapidly Around the World, but Not Always Equally. Pew Research Center. Retrieved from https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/
(2020). Social Determinants of Health. U.S. Department of Health and Human Services. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/access-to-health
Strunk, B., Cunningham, P. (2002). Treading Water: Americans’ Access to Needed Medical Care, 1997-2001. Washington, DC: Center for Studying Health System Change, Tracking Report 1. Retrieved from http://www.hschange.org/CONTENT/421/
(2018). Table 29. Delay or nonreceipt of needed medical care, nonreceipt of needed prescription drugs, or nonreceipt of needed dental care during the past 12 months due to cost, by selected characteristics: United States, selected years 1997–2017. Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/nchs/data/hus/2018/029.pdf
(2013). The Mobile Consumer, A Global Snapshot. Nielsen. Retrieved from
https://www.nielsen.com/wp-content/uploads/sites/3/2019/04/Mobile-Consumer-Report-2013-1.pdf
(2020). Wellvis COVID-19 Triaging App. The Wellviser Company. Retrieved from https://covid19.wellvis.org/
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.