
Previously on Screen the Lungs!, we discussed some of the challenges and barriers that cancer patients face in deciding whether lung cancer screening is right for them.
In today’s discussion, I want to talk more about how we can help patients navigate not only the initial decision to screen, but their entire cancer journey.
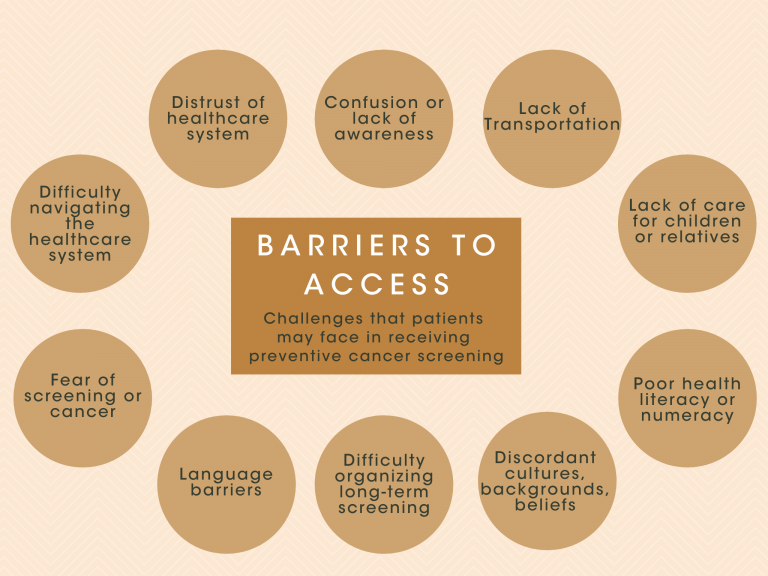
At any stage of cancer, every patient will have a unique experience that determines their ability to engage with their care. Inequalities in social position, economic status, culture, education, environment, and other social determinants of health are critical factors of their cancer experience. Many underserved, marginalized, or disadvantaged patients face barriers that prevent them from getting what they need.
Patient Navigation programs are designed to help address these barriers by supporting and guiding cancer patients longitudinally throughout their cancer journey, to mitigate barriers to receiving care at every step.
Trained Patient Navigators (PNs) act as liaisons that bridge many of the gaps that alienate patients by working with patients on an individual and personalized basis, answering questions, offering support, and ultimately acting as their compass through the cancer screening and care experience.
Since the 1990s, PN programs for various cancer diseases have seen great effectiveness, especially in preventive screening programs.

Across multiple cancer diseases, including lung cancer, screening programs with dedicated PN have demonstrated significantly increased screening use and adherence to annual screening programs. PN is also especially effective at reaching traditionally undeserved and marginalized patients, such as low-Socio-Economic Status (SES) groups and minority populations, thus, improving cancer care equity as well as longitudinal disease outcomes and health disparities.
A recent randomized trial studying lung cancer screening PN within communities of low SES strongly demonstrates the potential of PN specifically designed for lung cancer screening (LCS) programs. In this study, patients at 5 community health centers who were provided a novel patient navigation intervention saw an almost three times greater rate of LCS usage as compared to non-navigated patients.

While embedded healthcare professionals, such as nurse practitioners, make great PNs, non-professionals can also make a significant impact and vastly widen the ability of community health systems to develop navigation programs.
Any health system can look to its patient and cancer community to build PN networks. Typical non-health professional PNs that staff successful navigation programs are trained laypersons who are representatives of or have some connection to the cancer patient community. These community-based PNs may include cancer survivors, relatives of cancer patients, or those that share a community of identity with patients.
The shared lived experiences of such PNs with patients can allow them to make connections with their patients and cultivate a level of trust that patients may not have with other healthcare providers.
Effective PN for lung cancer must address three primary stages in the screening process:
The needs of cancer patients and their families are constantly shifting. Thus, Patient Navigation must be dynamic and flexible. To promote mindfulness and keep PN programs adaptive, PN programs should be constantly evaluated and refined to maximize the effectiveness of navigation practices, consider the evolving needs of patients, and propose new strategies for helping patients. The key metrics used to evaluate PN program success should include patient satisfaction, longitudinal outcomes, health equity, as well as time to diagnosis and treatment.
More from Brian Shim here.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.