
Welcome to my blog on “Advancing Black Feminism in Public Health.” My goal is to move black feminism from the margins to the center of public health by applying 10 key principles as legitimate and comprehensive frameworks for adequately addressing health threats and related social and structural determinants of health in the lives of black women and girls.
Dr. Quinn M. Gentry
In this blog, I highlight the significance of organizational change as fundamental to principle no. 6 (of 10): Frame change within the context of organizational, structural, and individual transformation in advancing black feminism in public health.
Organizational change refers to the systemic tasks needed to build capacity in key areas that increase organizational effectiveness. For public health, I focus on organizational capacity-building to enhance programs for better participant outcomes.
“Challenging power structures from the inside, working the cracks within the system...requires learning to speak multiple languages of power convincingly.”
Patricia Hills Collins, Black Feminist Thought Leader Tweet
Understanding organizations’ governing protocols, approach to personnel, policy guidelines, and partnership selection is crucial to implementing organizational change within public health initiatives. Once organizations are operating at full capacity, individuals participating in programs and services are better positioned to commit to the behavioral changes needed for optimal health outcomes.
As a public health program evaluator, I am deeply troubled by some administrators’ “blame the participant” narrative when programs fail to meet key performance measures. Armed with Hill Collins’ insistence that we challenge power structures from within, I integrated organizational performance measures into evaluation designs for diverse health programs funded at the federal, state, and foundation levels. This afforded me the opportunity to observe organizations’ effectiveness in program implementation using measures beyond individual change in behaviors. While it is beyond the scope of this blog to provide an exhaustive list, I have shared some organizational-level data pertaining to recurring themes about organizations’ limitations in program effectiveness.

The conceptual frameworks below contribute to the process of organizational change and are especially helpful in public health and social service agencies.
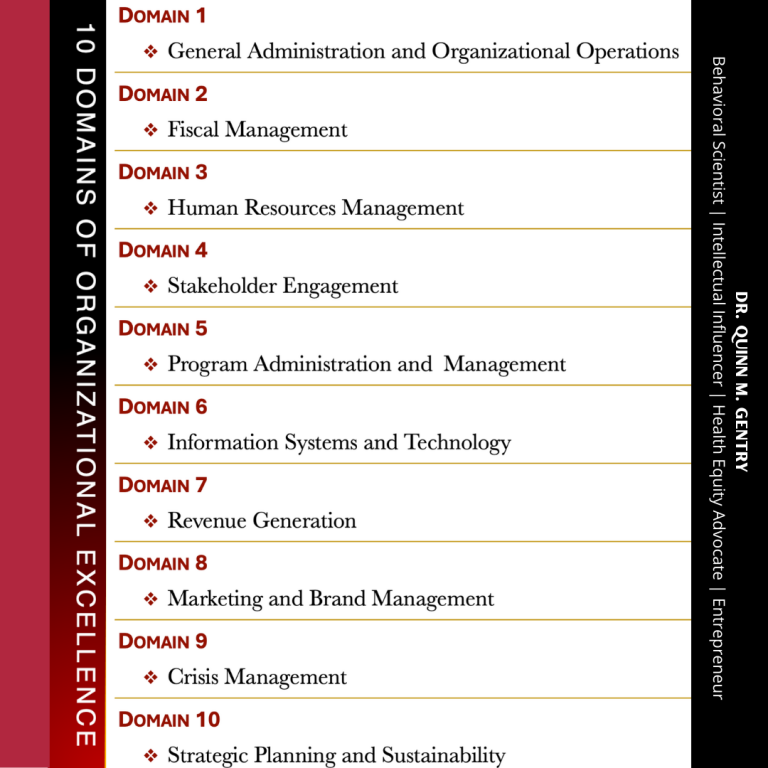
In advancing black feminism in public health, I built a body of work for assisting black women- and girls-serving organizations to achieve optimal levels of effectiveness. My working definition of “organizational effectiveness” is the intersection of efficacy (ability to achieve its mission, goals, and objectives) and efficiency (working within allotted resources). I operationalized my definition of organizational effectiveness into “10 domains of organizational excellence”. Each domain requires competent leadership and management for high organizational performance over long periods of time and should be an area of focus for improvement to achieve organizational excellence.

“Organizational Leadership is a contact sport: you really learn what matters most after you lead a team through a crisis with internal threats to your integrity and systems and external factors aiming missiles at all of your competitive advantages and resources.”
“Dr. Quinn, Intellectual Influencer Tweet
As black feminists advocating for health equity, we must be bold enough to challenge power structures from inside the public health and medical systems, as we observe cracks in the very systems and organizations funded to fix patients whose health is a matter of life and death. As bold, brilliant thought leaders, never lose sight of what MATTERS most in Public Health!

More by Dr. Quinn M. Gentry here.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.