Iyiegbuniwe E, Ufelle AC, Adams A. Occupational lead exposures among university police officers and instructors at an outdoor shooting range in Southcentral Kentucky. HPHR. 2021; 33.
DOI:10.54111/0001/GG9
There is a potentially high risk of lead exposure among police officers and instructors at an outdoor firing range. In the United States, occupational lead exposure remains an important and significant public health problem. Lead causes both acute and chronic adverse health effects in multiple human organ systems. The Occupational Safety and Health Administration (OSHA) has promulgated a Permissible Exposure Limit and Action Level of 50 µg/m3 and 30 µg/m3 for lead averaged over an 8-hour period, respectively (general industry standards). Excessive lead exposures have been previously reported in several studies that evaluated groups of firearm shooters and instructors at firing ranges. Many of those studies focused mainly on personal lead exposures at either indoor or covered outdoor firing ranges. The present study was conducted with a sample of 17 university police officers (14 shooters and 3 instructors) to assess their occupational lead exposures at an uncovered outdoor firing range in Bowling Green, Kentucky. The study occurred over a period of three days during the months of June and July. The results showed that personal exposures to lead ranged from a concentration of 5.5 to 146 µg/m3. In addition, personal exposures reported for some police officers significantly exceeded OSHA’s general industry lead standards, without consideration of the use of personal protective equipment. The use of copper-jacketed ammunition and personal protective equipment combined with adequate work practices are highly recommended for this group of police officers and instructors. The effective implementation of proactive control measures is necessary to reduce airborne lead levels and invariably minimize potential inhalation and absorption of lead by police officers at firing ranges.
Low-level Personal Lead Exposure, Lead Concentration, Police Officers, Firearm Instructors, Outdoor Shooting Range
The increased use and applications of lead in numerous industries is due to its abundance and unique physical and chemical properties (Maret, 2017; Koh, Locke, Chen, Purdue, & Friesen, 2015). According to the Agency for Toxic Substances and Disease Registry, ([ATSDR], 2020), historically, occupational lead exposure sources have included the manufacture of lead-based paints, pigments, and glazes; electrical shielding; plumbing; storage batteries; solder; welding fluxes; ammunitions; mining and smelting of ore; manufacture and application of lead-containing pesticides; combustion of coal and oil; and waste incineration. Other occupations in which workers may be potentially exposed to lead include, battery manufacturing, chemical industry, construction workers, demolition workers, firing range instructors, foundry workers, gas-station attendants, gasoline addictive production, jewelers, etc. (Staudinger & Roth, 1998). Although lead in gasoline and paint were banned in the United States, (Arnemo et al., 2016; Holland, Cawthon, & Levels, 2016), its use in ammunitions is still a major source of exposure (Arnemo et al., 2016).
In a recently published “Toxicological Profile for Lead” the ATSDR (2020) noted that depending on the particle size of lead, inhalation exposures are more important in occupational settings. In addition to inhalation, occupational exposure to organic lead compounds often involves dermal absorption. Regardless of the route of entry of lead into the body, the primary systemic toxic effects appear to the same. Lead exposure in adults is a major risk factor for death from cardiovascular diseases and significant lead poisoning is associated with elevated risks for chronic renal failure, hypertension and coronary heart disease, and premature death (ATSDR, 2020). Available case studies from the Agency for Toxic Substances and Disease Registry (ATSDR, 2020) have focused primarily on lead exposures and regulations in the United States. The health effects of lead in children of all races and ethnic origins is of public health significance since they are at greatest risks of lead poisoning (Hauptman, Bruccoleri, & Woolf, 2017; Lin et al., 2019). Additionally, in children, lead is a known neurotoxin that causes severe and irreversible neurological harm, growth and developmental retardation, reduced intelligent quotient and academic abilities, and behavioral problems (Benfer et al., 2020). Currently, there is no safe threshold for blood lead level (BLL) in children because BLLs once considered safe have been demonstrated to be unhealthy and of significant public health importance (ATSDR, 2020).
There is considerable adverse health effects of occupational lead exposure in adults, particularly those who work in industries with high lead exposures (Arnemo et al., 2016). Lead is known to affect every organ in the human body and remains one of the most commonly found hazards at Superfund sites in the United States. Lead may cause irreversible neurological damage as well as renal disease, cardiovascular effects, and reproductive toxicity. The nervous, cardiovascular, reproductive, immune, and gastrointestinal systems as well as the kidneys are particularly targeted for lead toxicity (Koh et al., 2015). In a nationally representative sample of 14,289 United States adults aged 20 years or older, Lanphear et al. (2018) showed that a total of 4,422 people deaths (1801 or 38% from cardiovascular disease and 988 or 22% from ischaemic heart disease). The study further showed that an increase in the concentration of blood lead from 1.0 μg/dL to 6.7 μg/dL was associated with all-cause mortality, cardiovascular disease mortality, and ischaemic heart disease mortality.
There is sufficient evidence that BLLs<10µg/dL may be associated with essential tremor, hypertension, cardiovascular-related mortality, electro-cardiovascular abnormalities and impaired kidney function. Furthermore, there is evidence that elevated BLLs are associated with reduced fetal growth in pregnant women, limited evidence of associated decreased hearing and cognitive functions, and incidence of amyotrophic lateral sclerosis (Laidlaw, Filippelli, Mielke, Gulson, & Ball, 2017). Furthermore, inorganic lead is classified by the International Agency for Research on Cancer ([IARC], 2006) as a Group 2A carcinogen with the increased probability of being carcinogenic to humans (Rousseau, Straif, & Siemiatycki, 2005).
Shooting ranges are often used by professionals, including police officers who are required to maintain certain levels of firearm proficiency and by other individuals for recreational purposes. A study by Beaucham et al. (2014) reported that approximately one million law enforcement officers trained at 18,000 indoor shooting ranges in 2014. (Beaucham et al., 2014). It is widely known that lead is a major component of ammunitions since the bullet projectile and primer often contain lead styphnate and lead peroxide (Johnson-Arbor, Soto, & Liu, 2020). As a result, firearm operators may be exposed to high levels of lead depending on the type of ammunition, duration of exposures, and frequency of firearm use. Available research suggests a strong positive correlation between the frequency of shooting and reported BLLs, with higher shooting frequency corresponding to higher BLLs (Laidlaw et al., 2017). Furthermore, inhalation exposure during shooting is influenced by not only the type of ammunition but the amount of ventilation and prevailing conditions in open and indoor shooting ranges (Grandahl, Suadicani, & Jacobsen, 2012).
Lead ammunition is still widely used at shooting ranges and other gun-related activities and is perhaps the most significant unregulated source of intentional release of lead into the environment (Bellinger et al., 2013). Indoor shooting range is a significant source of lead exposure among users and elevated blood lead levels were recorded among workers at a recreational indoor firing range (Demmeler, Nowak, & Schierl, 2009). A study of Brazilian police officers who participated in a yearly mandatory shooting exercises in indoor shooting range showed high levels of lead exposures with mean pre- and post- exposure BLLs of 3.3 μg/dL ± 0.15 and 18.2 μg/d L± 1.5, respectively(Rocha, Sarkis, Carvalho Mde, Santos, & Canesso, 2014). In addition, lead accumulation in the surrounding soil at an outdoor firing range is another source of lead exposure among shooters (Hardison, Ma, Luongo, & Harris, 2004; Laidlaw et al., 2017). It is also important to note that lead contamination of the soil in an outdoor shooting range can result in underground water contamination that threatens the environment (Mariussen et al., 2017).
In the United States, several lead standards and guidelines have been promulgated by the Occupational Safety and Health Administration (OSHA), the National Institute for Occupational Safety and Health (NIOSH), and the American Conference of Governmental Industrial Hygienists (ACGIH®). OSHA’s general industry lead standard was promulgated on November 14, 1978 and applies to all occupational lead exposures except those in construction and agriculture. The current eight-hour permissible exposure limit (PEL) and action level (AL) for occupational lead exposures (29 CFR 1910.1025) are 50µ/m3 and 30µ/m3, respectively (OSHA, 1978). OSHA’s lead standards require that workers be removed from lead exposure when BLLs are ≥ 50µg/dL (construction workers) or ≥ 60µg/dL (general industries) and workers are allowed to return to work at BLLs <40µg/dL (Holland et al., 2016).
Engineering controls such as the use of local exhaust ventilation and enclosure are required to control airborne lead exposures in the workplace. In addition, stringent control measures including process enclosures are recommended to control lead in the workplace. When required, respirators must be implemented in accordance with 29 CFR 1910.134 (OSHA, 1978). Also, the employer must institute a medical surveillance program that is administered by a licensed physician for all employees potentially exposed at or above the AL of 30 μg/m3. Furthermore, the National Institute for Occupational Safety and Health (NIOSH) has recommended an acceptable BLL of 5µg/dL and values above this level are considered elevated BLLs (NIOSH, 2021). The American Conference of Governmental Industrial Hygienists (ACGIH) also recommends a Threshold Limit Value (TLV) of 50 μg/m3 for lead as an 8-hour TWA. The ACGIH classifies lead as a confirmed animal carcinogen with unknown relevance to humans.
Lead poisoning is a completely preventable disease. Primary prevention is the most important and significant strategy to protect children and adults from lead poisoning (ATSDR, 2020).
Although most of the previous studies have focused primarily on lead exposures in indoor shooting ranges, there exists a paucity of information on lead exposures at outdoor shooting ranges. A recent noise exposure study of the same group of university police officers (i.e., included in this study) during their qualification courses at an outdoor shooting range showed exposures to elevated noise levels with the potential for long-term noise-induced hearing loss and other health effects (Iyiegbuniwe, Ufelle, & Britt, 2019). This present study provides an evaluation of airborne personal lead concentrations for 17 police officers and 2 instructors during firearm (handgun and rifle) qualifications (annual training) at an outdoor shooting range in Southcentral Kentucky. Additionally, the study was conducted to determine if lead exposures of the police officers and instructors were in compliance with applicable OSHA lead standards. This is with a view to promoting safer work-practices and protecting the health of police officers and their instructors during future firearms qualifying courses.
Personal lead exposure monitoring was conducted over a three-day period among 19 police officers including 17 trainees and 2 instructors at a regional university in Southcentral Kentucky to measure exposure to airborne lead at an outdoor firearms training center.
The tasks and activities involved shot gun and rifle qualification courses that evaluated the accuracy and speed of police officers as they shot at various targets from pre-designated distances while standing, kneeling and lying down. The police officers participated in a practice course immediately prior to the qualification course. The distances, rounds of ammunition fired, and allotted time were the same for both the practice and qualification course. During the handgun course, trainees fired a total of 50 rounds of ammunition from pre-designated distances of 2, 5, 7, 15, and 25 yards. Similarly, during the rifle course, trainees fired a total of 50 rounds using 45 rifles and 5 pistols from pre-designated distances of 7, 15, 25, 35, and 50 yards. In addition, trainees fired from different positions including standing, prone, and kneeling. Prior to the qualification courses, the instructor provided lead awareness training to the police officers. Topics covered included sources of occupational lead exposure, the health effects of lead, steps to minimize lead exposures, and applicable lead standards and regulations. Copies of OSHA’s Lead Standard (CFR 1910.1025) and its applicable Appendices were made available to the police officers and instructors who participated in the handgun and rifle qualifications.
Airborne lead samples were collected in accordance with NIOSH Method 7300 (National Institute for Occupational Health and Safety, 2003).Samples were collected using 37-mm mixed cellulose ester membrane filter cassettes (0.8-μm pore size) attached to personal sampling pumps calibrated within ± 5% of the recommended flow rate of 2 liters per minute. Personal lead samples were collected under conditions that were representative of each trainee’s daily exposure. For the handgun qualification course, the sampling times ranged from 18 to 228 minutes and the sample volumes ranged from 45 to 297 liters and for the rifle qualifications, the sampling times ranged from 58 to 202 minutes and the volumes ranged from 145 to 272 liters.
All sampling pumps with in-line filters were allowed to run continuously during each day’s qualifications for determination of time weighted average (TWA) concentrations. Field blanks were prepared for quality control purposes and together with the samples and corresponding chain of custody forms were shipped to a certified American Industrial Hygiene Laboratory for analysis.
Sample analysis was conducted at an accredited laboratory in accordance with NIOSH Method 7300 using inductively coupled plasma-atomic emission spectrometer that was equipped for inorganic lead analysis. Lead concentrations below the laboratory analytical detection limits were treated as being equivalent to zero. Using the air volume sampled and the laboratory result for each personal air sample, we calculated the 8-hour TWA concentration of lead (mg/m3). Additionally, statistical data analysis was conducted using T-test for the comparison of means of actual and calculated lead concentrations obtained during both handgun and rifle qualifications. All data with p-values ≤ 0.05 were considered to be significant (GraphPad Prism, version 7.05, San Diego, CA 92108, www.graphpad.com).
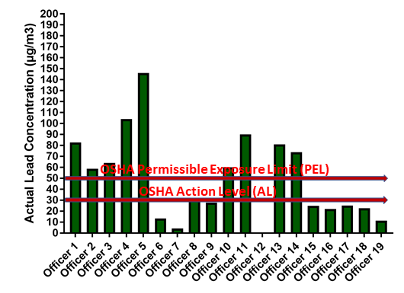
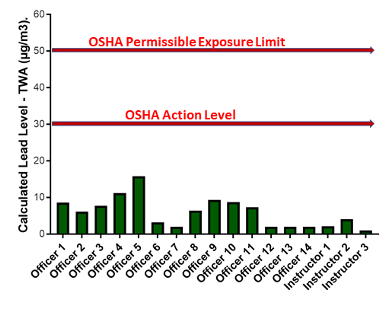
The actual results of personal lead exposure levels for police officer during both the handgun and rifle qualifications are shown in Tables 2 and 3 and summarized in Figures 2-4 below. For handgun qualifications, the average personal lead concentrations ranged from 5.5 to 146 µg/m3 (Table 1, Figure 2). The calculated lead levels based on 8-hour time-weighted average concentrations ranged from 2.0 to 15.8 µg/m3 (Table 2, Figure 3) and these were well below both the PEL and AL of 50 µg/m3 and 30 µg/m3, respectively.
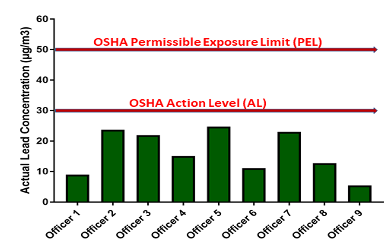
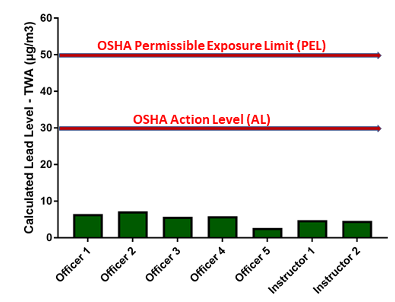
The results of actual sampled personal lead exposure levels for police officers during rifle qualifications ranged from 5.6 to 24.7 µg/m3 (Table 3, Figure 4). Furthermore, the calculated lead levels as 8-hour TWA concentrations ranged from 2.7 to 7.2 µg/m3 (Table 4, Figure 5) and these were well below both the PEL and AL.
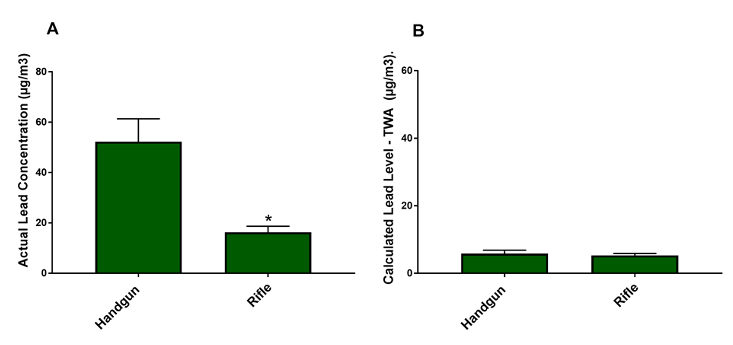
The results showed a significant difference between actual (sampled) personal lead exposures for all police officers during handgun qualifications when compared with rifle qualifications (Figure 6). However, there was no significant difference between the calculated 8-hour TWA concentrations between handgun and rifle.
In this study, the actual sampling results indicated that some of the police officers and their instructors were exposed to lead levels above the OSHA PEL and AL during the firearm qualification course. This resulted in further assessment to determine the extent of exposures among police officers and instructors. As shown in Table 1 and summarized in Figure 2, the actual lead exposure from handgun ranged from 5.5 to 146 µg/m3 () while the corresponding calculated 8-hour TWA were below both the OSHA PEL and AL (Table 2, Figure 3). In addition, we observed that the lead exposures during rifle qualifications ranged from 5.56 to 24.7 µg/m3 (Table 3, Figure 4) and the calculated 8-hour TWA for lead exposure were also below the OSHA PEL and AL (Table 4, Figure 5). Considering the fact that this qualification course occurred within a short period of time, typically once every year, the affected police officers would be far less likely to be overexposed to lead when compared to their instructors who repeat the process during various times throughout the year and hence spent more times at the shooting range.
In a previous study that used police officers as controls and compared lead exposures at multiple shooting ranges, blood lead levels among the different groups of exposed individuals were reported above the reference values Also, instructors had the highest levels of lead when compared to special forces and shooting range maintenance staff, (Vandebroek, Haufroid, Smolders, Hons, & Nemery, 2019). Despite the fact that the observed lead levels in our study are below OSHA lead standards, a number of recent studies have demonstrated that increasing cardiovascular mortality risk have occurred at lower levels of lead than previously reported (Arnemo et al., 2016; Lanphear, 2018).
In support of our data, a previously published review article indicated that instructors are at risk for excessive exposure to lead during shooting exercises (Fischbein, 1992). Lead exposure levels are affected my multiple factors such are age, job seniority or length of service, age, and types of occupation (Di Lorenzo et al., 2010). Users of indoor shooting ranges especially members of the military are often exposed to elevated lead levels that can potentially cause adverse health effects (Park, Lee, Lee, Yoon, & Moon, 2016). Furthermore, it has been shown that at indoor shooting ranges, the airborne lead levels were usually above the internationally adopted lead standards and that trainees had higher BLLs when compared to their instructors. Furthermore, amino levulinic acid dehydrogenase (ALAD), an indicator of lead activity was significantly lower when compared to a control group (Abudhaise et al., 1996).
Similar to our findings, another study found that firearm instructors in both indoor and outdoor shooting ranges were exposed to lead levels below the ACGIH‘s Biological Exposure Indices (Di Lorenzo et al., 2010). Another study showed that a high school coach for a shooting team had significantly elevated BLL and that 66 team members were equally exposed to elevated lead levels (Centers for Disease & Prevention, 2005). This supports the disparity in exposures that occur between instructors and their trainees. Similar to the instructors, shooting range employees often spend increased number of hours at indoor ranges and are exposed to elevated levels of lead when compared to the trainees and other individuals (Kang & Park, 2017). Another related study on outdoor shooting range that involved military officers, indicated that there is a higher probability of trainees being exposed to lead levels above the OSHA’s AL for lead when compared to instructors, thus indicating that exposure disparity exists between the two groups (Greenberg, Frimer, Meyer, Derazne, & Chodick, 2016).
Our results indicated that there is significant difference between actual lead exposures during handgun and rifle qualifications, but none for calculated 8-hour TWA (Figure 6). This suggests that there may be subtle differences in lead exposure between handgun and rifle. In essence, the caliber of ammunitions may play a role in the amount of lead exposure (Laidlaw et al., 2017), as shooters with large caliber weapons and ammunitions often have higher BLLs compare to shooters with smaller caliber weapons (Johnson-Arbor et al., 2020).There are numerous adverse health effects associated with lead exposure involving the use of firearms at shooting ranges and in other professional and recreational activities. A South African study indicated that there is an association between lead exposure in shooting ranges and the development of aggressive behaviors at BLLs of ≥10µg/dL (Naicker, de Jager, Naidoo, & Mathee, 2018) and that at low lead blood levels, there is an association with neuropsychiatric symptoms and miscarriage in partners of the shooters (Aguilar Madrid et al., 2016). Furthermore, there is an indication that verbal memory may be impaired in sports involving shooters due to lead exposures (Asa-Makitaipale, Jehkonen, Uitti, & Vilkki, 2009). As a result of the health effects of lead exposure even at lower levels (Shaffer & Gilbert, 2018), there is need to adopt preventive measure to protect police officers during handgun and rifle qualifications.
A previous study (Tripathi, Sherertz, Llewellyn, Armstrong, & Ramsey, 1990) indicated that using totally copper-jacketed ammunitions at a covered outdoor shooting range significantly reduced airborne lead levels in the breathing zone of the shooters. . Additionally, lead exposures in the shooting range can be controlled by substitution with lead free bullets, use of adequate ventilation system, and the use of wet mopping or HEPA vacuuming in place of dry sweeping (Beaucham et al., 2014). Periodic monitoring of BLL of police officers in the firing ranges will go a long way in minimizing the risks of high lead exposures.
As detailed in Appendixes A and B of OSHA’s General Industry Standard for Lead (29 CFR 1910.1025), training is mandatory whenever employees are potentially exposed to high airborne levels of lead. Among other things, the standard stipulates that employees be monitored to determine their personal exposures to airborne lead during a full work-shift of 7 or more continuous hours (OSHA, 1978). Lead monitoring must occur during every shift of potential personal exposures to lead and without regard to the use of respiratory protection by the affected employees. Subsequently, if the data showed that personal exposures were below the AL (30 μg/m3), OSHA requires that all lead exposure results must be documented in writing, hence requires no additional monitoring. However, when personal lead exposure levels exceed the AL but below the PEL, affected employers must conduct additional personal lead monitoring every 6 months until such a time when two consecutive lead measurements (sampled at least 7 days apart) were below the AL. Additionally, all personal lead exposure results that exceeded OSHA’s PEL would require that the employer conduct continuous personal lead exposure monitoring every 3 months or calendar quarters.
Finally, the lead standard stipulates that when two consecutive measurements (sampled at least 7 days apart) fall below the PEL, then the monitoring frequency can be reduced to every 6 months only (OSHA, 1978). It must be noted that NIOSH had previously published a Federal Register notice in 1997 requesting public comments and information regarding potential health risks associated with inorganic lead exposures at or below the OSHA PEL of 50 μg/m3in occupational settings. However, no additional actions have been taken and no new recommended guidelines have been proposed for lead to-date by the agency.
One of the limitations of this study is that this study was conducted over a 3-day period during the summer and potential seasonal variations in exposure may occur. Additionally, this study focused primarily on airborne personal lead exposures and did not account for other potential sources of lead exposures, including, but not limited to surface lead in the surrounding soil. Because of the short duration of the study, no attempt was made to monitor for BLLs of the police officers before and after the firearms qualification courses. Determination of BLLs during firearm qualification courses is important for detecting police officers who may be potentially at higher risks of adverse health effects from lead poisoning. Finally, the duration of shooting was limited and may not be sufficient time to adequately understand the full extent of exposures and the long-term implications of lead concentrations determined during this study. A future study that involves more comprehensive and all-year round monitoring of all university police officers and instructors who may be potentially exposed to high lead levels at the shooting range is recommended. Finally, it will be impactful and informative if future studies are designed to incorporate longer sampling durations and be conducted at both indoor and outdoor shooting ranges during different seasons of the year.
In this study, we evaluated occupational lead exposures among 19 university police officers during handgun and rifle qualifications. The study occurred over a three-day period in summer at an uncovered outdoor shooting range in Southcentral Kentucky. Lead samples were collected using 37-mm mixed cellulose ester membrane filter cassettes (0.8-μm pore size) attached to personal sampling pumps calibrated at 2 liters per minute. Laboratory analysis for inorganic lead analysis was conducted in accordance with NIOSH Method 7300 using inductively coupled plasma-atomic emission spectrometer. The results showed that personal lead exposures ranged from 5.5 to 146 µg/m3 and 2.0 to 15.8 µg/m3 for actual and calculated 8-hour TWA, respectively. Without consideration of respiratory protection, some actual police officers’ exposures would have significantly exceeded the OSHA’s lead standards. The results further showed that there is a significant difference in actual personal lead exposures during handgun qualifications when compared to rifle qualifications, suggesting that the caliber of weapon and the ammunitions used may be factors that are important in assessing lead exposures at an outdoor shooting range. It must be noted that, without regard to the use of respiratory protection and duration of exposures in the affected police officers and their instructors, low levels of lead exposures were determined and some actual concentrations exceeded both the PEL (50 μg/m3) and AL(30 μg/m3). However, the results of calculated 8-hour TWA concentrations showed that personal lead exposures were well below both the PEL and AL. As required by OSHA, all lead exposure results must be documented in writing and lead monitoring is recommended during every qualification course. Available evidence suggests that significant health effects may be associated with low levels of lead, including cardiovascular disease mortality in adults. Lead poisoning is a completely preventable disease and primary prevention is the recommended public health strategy for protection of children and adults against lead poisoning. To reduce lead exposures and prevent potential cardiovascular diseases and other documented health effects of lead, a comprehensive public health strategy including the use of copper-jacketed ammunitions combined with adequate personal protective equipment and good work practices are highly recommended for these police officers.
Table 1: Sampled Personal Lead Concentrations of Police Officers during Handgun Qualifications
Sample ID | Sampled Lead Concentration (µg/m3) |
Officer 1 |
82.6 |
Officer 2 | 58.6 |
Officer 3 | 64.1 |
Officer 4 | 104.0 |
Officer 5 | 146.0 |
Officer 6 | 13.3 |
Officer 7 | 4.3 |
Officer 8 | 30.2 |
Officer 9 | <27.8 |
Officer 10 | 59.9 |
Officer 11 | 90.1 |
Officer 12 | N/A |
Officer 13 | 80.9 |
Officer 14 | 73.7 |
Officer 15 | <25.0 |
Officer 16 | 22.0 |
Officer 17 | 25.0 |
Officer 18 | 22.7 |
Officer 19 | 11.4 |
OSHA PEL = 50 µg/m3, AL = 30 µg/m3
Table 2: Calculated Personal Lead Concentrations of Police Officers (as 8-hour TWA) during Handgun Qualifications
Sample ID | Calculated Lead Concentrations (µg/m3) |
Officer 1 | 8.6 |
Officer 2 | 6.1 |
Officer 3 | 7.7 |
Officer 4 | 11.2 |
Officer 5 | 15.8 |
Officer 6 | 3.2 |
Officer 7 | 2.0 |
Officer 8 | 6.4 |
Officer 9 | 9.3 |
Officer 10 | 8.7 |
Officer 11 | 7.3 |
Officer 12 | 2.0 |
Officer 13 | 2.0 |
Officer 14 | 2.0 |
Instructor | 2.1 |
Instructor | 4.1 |
Instructor | 1.0 |
OSHA PEL = 50 µg/m3, AL = 30 µg/m3
Table 3: Sampled Personal Lead Concentrations of Police Officers during Rifle Qualifications
Sample ID | Sampled Lead Concentrations (µg/m3). |
Officer 1 | 9.0 |
Officer 2 | 23.7 |
Officer 3 | 21.9 |
Officer 4 | 15.1 |
Officer 5 | 24.7 |
Officer 6 | 11.1 |
Officer 7 | 23.0 |
Officer 8 | 12.7 |
Officer 9 | 5.5 |
Officer 10 | N/A |
OSHA PEL = 50 µg/m3, AL = 30 µg/m3
Table 4: Calculated Personal Lead Concentrations of Police Officers (as 8-hour TWA) during Rifle Qualifications
Sample ID | Calculated Lead Concentrations (µg/m3) |
Officer 1 | 6.5 |
Officer 2 | 7.2 |
Officer 3 | 5.7 |
Officer 4 | 5.8 |
Officer 5 | 2.7 |
Instructor | 4.8 |
Instructor | 4.6 |
OSHA PEL = 50 µg/m3, AL = 30 µg/m3

Abudhaise, B. A., Alzoubi, M. A., Rabi, A. Z., & Alwash, R. M. (1996). Lead exposure in indoor firing ranges: environmental impact and health risk to the range users. Int J Occup Med Environ Health, 9(4), 323-329.
Agency for Toxic Substances and Disease Registry. (2020). Toxicological Profile for Lead. Retrieved from https://www.atsdr.cdc.gov/toxprofiles/tp13-p.pdf
Aguilar Madrid, G., Tellez-Cardenas, L., Juarez-Perez, C. A., Haro-Garcia, L. C., Mercado-Garcia, A., Gopar-Nieto, R., & Cabello-Lopez, A. (2016). Blood lead determinants and the prevalence of neuropsychiatric symptoms in firearm users in Mexico. Int J Occup Med Environ Health, 29(2), 219-228. doi:10.13075/ijomeh.1896.00358American Conference of Governmental Industrial Hygienists (ACGIH). (2020). 2020 TLVs® and BEIs®. American Conference of Governmental Industrial Hygienists, Cincinnati, OH
Arnemo, J. M., Andersen, O., Stokke, S., Thomas, V. G., Krone, O., Pain, D. J., & Mateo, R. (2016). Health and Environmental Risks from Lead-based Ammunition: Science Versus Socio-Politics. Ecohealth, 13(4), 618-622. doi:10.1007/s10393-016-1177-x
Asa-Makitaipale, S., Jehkonen, M., Uitti, J., & Vilkki, J. (2009). Memory functions in recreational pistol sport shooters: does lead matter? Environ Health Insights, 3, 13-18. doi:10.4137/ehi.s894
Beaucham, C., Page, E., Alarcon, W. A., Calvert, G. M., Methner, M., Schoonover, T. M., . . . Prevention. (2014). Indoor firing ranges and elevated blood lead levels – United States, 2002-2013. MMWR Morb Mortal Wkly Rep, 63(16), 347-351.
Bellinger, D. C., Burger, J., Cade, T. J., Cory-Slechta, D. A., Finkelstein, M., Hu, H., . . . Smith, D. R. (2013). Health risks from lead-based ammunition in the environment. Environ Health Perspect, 121(6), A178-179. doi:10.1289/ehp.1306945
Benfer, E. A., Coffey, E., Gold, A. E., Hanna-Attisha, M., Lanphear, B. P., Li, H. Y., . . . Walz, K. (2020). Health Justice Strategies to Eradicate Lead Poisoning: An Urgent Call to Action to Safeguard Future Generations. Yale Journal of Health Policy, Law, and Ethics, 19(2), 66.
Centers for Disease Control and Prevention. (2005). Lead exposure from indoor firing ranges among students on shooting teams–Alaska, 2002-2004. MMWR Morb Mortal Wkly Rep, 54(23), 577-579.
Demmeler, M., Nowak, D., & Schierl, R. (2009). High blood lead levels in recreational indoor-shooters. Int Arch Occup Environ Health, 82(4), 539-542. doi:10.1007/s00420-008-0348-7
Di Lorenzo, L., Borraccia, V., Corfiati, M., Mantineo, G. A., Caciari, T., Marino, M., & Soleo, L. (2010). Lead exposure in firearms instructors of the Italian State Police. Med Lav, 101(1), 30-37.
Fischbein, A. (1992). Lead poisoning: I. Some clinical and toxicological observations on the effects of occupational lead exposure among firearms instructors. Isr J Med Sci, 28(8-9), 560-572.
Grandahl, K., Suadicani, P., & Jacobsen, P. (2012). Individual and environmental risk factors for high blood lead concentrations in Danish indoor shooters. Dan Med J, 59(8), A4488.
Greenberg, N., Frimer, R., Meyer, R., Derazne, E., & Chodick, G. (2016). Lead Exposure in Military Outdoor Firing Ranges. Mil Med, 181(9), 1121-1126. doi:10.7205/MILMED-D-15-00454
Hardison, D. W., Jr., Ma, L. Q., Luongo, T., & Harris, W. G. (2004). Lead contamination in shooting range soils from abrasion of lead bullets and subsequent weathering. Sci Total Environ, 328(1-3), 175-183. doi:10.1016/j.scitotenv.2003.12.013
Hauptman, M., Bruccoleri, R., & Woolf, A. D. (2017). An Update on Childhood Lead Poisoning. Clin Pediatr Emerg Med, 18(3), 181-192. doi:10.1016/j.cpem.2017.07.010
Holland, M. G., Cawthon, D., & Levels, A. T. F. o. B. L. (2016). Workplace Lead Exposure. J Occup Environ Med, 58(12), e371-e374. doi:10.1097/JOM.0000000000000928
Iyiegbuniwe, E., Ufelle, A., & Britt, A. (2019). Noise Exposure Assessment for University Police Officers during Rifle and Shotgun Qualifications. Athens Journal of Health & Medical Sciences, 6(1), 18.
Johnson-Arbor, K., Soto, P., & Liu, L. (2020). Adult lead exposure from ammunition reloading and indoor residential shooting. Am J Ind Med, 63(8), 733-737. doi:10.1002/ajim.23119
Kang, K. W., & Park, W. J. (2017). Lead Poisoning at an Indoor Firing Range. J Korean Med Sci, 32(10), 1713-1716. doi:10.3346/jkms.2017.32.10.1713
Koh, D. H., Locke, S. J., Chen, Y. C., Purdue, M. P., & Friesen, M. C. (2015). Lead exposure in US worksites: A literature review and development of an occupational lead exposure database from the published literature. Am J Ind Med, 58(6), 605-616. doi:10.1002/ajim.22448
Laidlaw, M. A., Filippelli, G., Mielke, H., Gulson, B., & Ball, A. S. (2017). Lead exposure at firing ranges-a review. Environ Health, 16(1), 34. doi:10.1186/s12940-017-0246-0
Lanphear, B. P., Rauch, S., Auinger, P., Allen, R. W., & Hornung, R. W. (2018). Low-level lead exposure and mortality in US adults: a population-based cohort study. Lancet Public Health, 3(4), e177-e184. doi:10.1016/S2468-2667(18)30025-2
Lin, Y., Huang, L., Xu, J., Specht, A. J., Yan, C., Geng, H., . . . Hu, H. (2019). Blood lead, bone lead and child attention-deficit-hyperactivity-disorder-like behavior. Sci Total Environ, 659, 161-167. doi:10.1016/j.scitotenv.2018.12.219
Maret, W. (2017). The Bioinorganic Chemistry of Lead in the Context of Its Toxicity. Met Ions Life Sci, 17. doi:10.1515/9783110434330-001
Mariussen, E., Heier, L. S., Teien, H. C., Pettersen, M. N., Holth, T. F., Salbu, B., & Rosseland, B. O. (2017). Accumulation of lead (Pb) in brown trout (Salmo trutta) from a lake downstream a former shooting range. Ecotoxicol Environ Saf, 135, 327-336. doi:10.1016/j.ecoenv.2016.10.008
Naicker, N., de Jager, P., Naidoo, S., & Mathee, A. (2018). Is There a Relationship between Lead Exposure and Aggressive Behavior in Shooters? Int J Environ Res Public Health, 15(7). doi:10.3390/ijerph15071427
National Institute for Occupational Health and Safety. (2003). ELEMENTS by ICP 7300 (Nitric/Perchloric Acid Ashing). Retrieved from www.cdc.gov/niosh/docs/2003-154/pdfs/7300.pdf
Occupational Safety and Health Administration (OSHA). (1978). Occupational Safety and Health Standards Lead (Vol. 1910.1025).
Park, W. J., Lee, S. H., Lee, S. H., Yoon, H. S., & Moon, J. D. (2016). Occupational Lead Exposure from Indoor Firing Ranges in Korea. J Korean Med Sci, 31(4), 497-501. doi:10.3346/jkms.2016.31.4.497
Rocha, E. D., Sarkis, J. E., Carvalho Mde, F., Santos, G. V., & Canesso, C. (2014). Occupational exposure to airborne lead in Brazilian police officers. Int J Hyg Environ Health, 217(6), 702-704. doi:10.1016/j.ijheh.2013.12.004
Rousseau, M. C., Straif, K., & Siemiatycki, J. (2005). IARC carcinogen update. Environ Health Perspect, 113(9), A580-581. doi:10.1289/ehp.113-1280416
Shaffer, R. M., & Gilbert, S. G. (2018). Reducing occupational lead exposures: Strengthened standards for a healthy workforce. Neurotoxicology, 69, 181-186. doi:10.1016/j.neuro.2017.10.009
Staudinger, K. C., & Roth, V. S. (1998). Occupational lead poisoning. Am Fam Physician, 57(4), 719-726, 731-712.
The National Institute for Occupational Safety and Health (NIOSH). (2021). Adult Blood Lead Epidemiology and Surveillance (ABLES). Retrieved from https://www.cdc.gov/niosh/topics/ables/ReferenceBloodLevelsforAdults.html
Tripathi, R. K., Sherertz, P. C., Llewellyn, G. C., Armstrong, C. W., & Ramsey, S. L. (1990). Reducing exposures to airborne lead in a covered, outdoor firing range by using totally copper-jacketed bullets. Am Ind Hyg Assoc J, 51(1), 28-31. doi:10.1080/15298669091369286
Vandebroek, E., Haufroid, V., Smolders, E., Hons, L., & Nemery, B. (2019). Occupational Exposure to Metals in Shooting Ranges: A Biomonitoring Study. Saf Health Work, 10(1), 87-94. doi:10.1016/j.shaw.2018.05.006
Emmanuel A. Iyiegbuniwe, PhD, MSPH, MBA is Associate Professor of Public Health at the College of Education, Health and Human Services, at California State University, in San Marcos, CA.
Dr. Emmanuel Iyiegbuniwe earned both MSPH and PhD degrees in Environmental and Occupational Health Sciences from University of Illinois at Chicago and MBA from Western Kentucky University. He is an Associate Professor of Public Health at California State University San Marcos (CSUSM) and has over 28 years of academic, administrative, and consulting experience. He served as the inaugural Director for the MPH program at CSUSM with concentrations in Global Health and Health Promotion and Education where he provided vision and leadership.
Alexander Chukwuma Ufelle, MBBS, MPH, PhD is a physician, public health expert, and toxicologist with research interest in environmental and occupational health. He teaches is the teach in the MPH program at Slippery Rock University with emphasis on toxicology, and environmental and occupational health science. His overall goal is to maximize the interconnection between bench research work and public health practice in the area of lung diseases/air pollution, water pollution, and liver diseases.
Anita A. Adams, MHA, RS, CIEC has worked as a public health professional for over 18 years. She focuses on campus safety, indoor air quality and various public health related issues. She earned both a BS and MHA from WKU and holds certification as a Registered Sanitarian with the Commonwealth of Kentucky and a Council-certified Indoor Environmental Consultant. Environmental Air Quality Specialist, in Environmental Health and Safety, at Western Kentucky University, in Bowling Green, KY.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.