The menopause is a natural part of the female life cycle. But why do women become invisible after the menopause? Dr Jen Gunter answers my question 'Ain't I A Woman?"

A cervical cancer diagnosis is devastating for womxn, families, and society at large. Womxn are commonly diagnosed in their mid-40s, at the peak of their economic productivity, when they may have roles as primary caregivers. Collectively they lose almost 9 million years of their lives from premature death and disability due to cervical cancer (8.96 million Disability Adjusted Life Years).
In 2020 341,831 womxn died and almost twice as many were newly diagnosed with cervical cancer globally. More womxn die of cervical cancer today than pregnancy-related conditions. Following concerted global efforts, maternal deaths decreased by over one-third between 2000 and 2017. Thus, it is a true tragedy that some mothers survive pregnancy only to die of cervical cancer.
One woman dies of cervical cancer every two minutes. Each one is a tragedy, and we can prevent it
Dr Tedros Adhan Ghebreyesus, Director General World Health Organisation (WHO) Tweet
A cervical cancer death is a maternal death because women are not mothers only during childbirth. Investing in surgical capacity for comprehensive management of cervical cancer is investing in maternal health.
Professor Emmanuel Makasa, Leadership Team, Global Surgery Foundation (GSF) Tweet
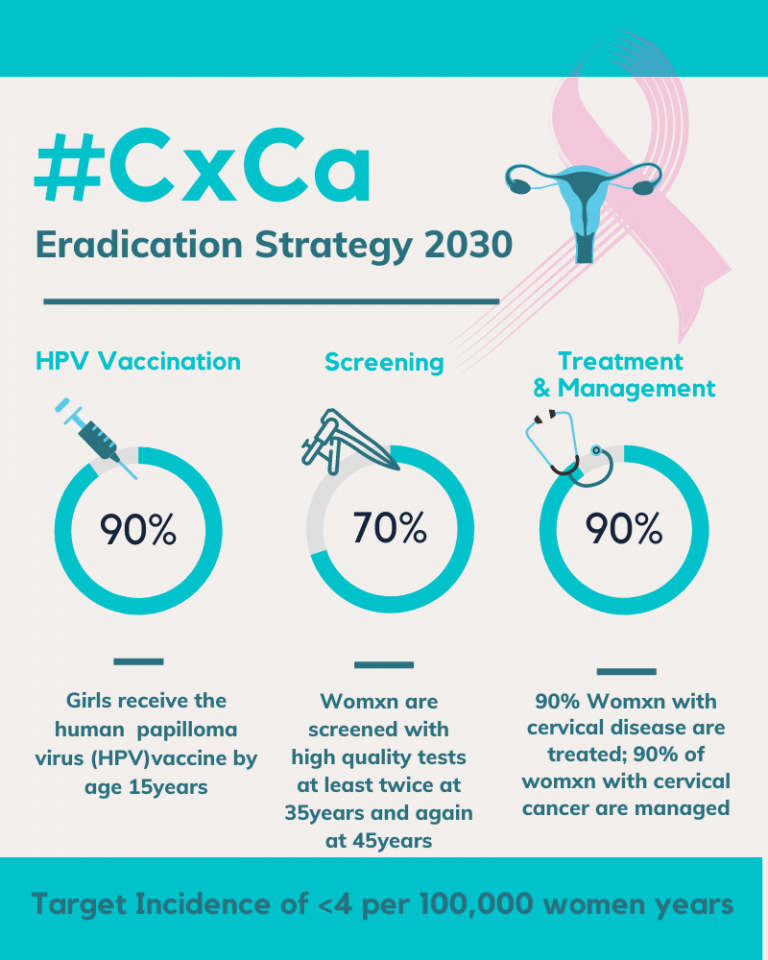
Cervical cancer is preventable and curable when detected early. In 2018, the World Health Organisation (WHO) raised a global call to action with the WHO Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. For countries to successfully eliminate cervical cancer as a public health problem, countries must have an incidence of fewer than 4 cases of cervical cancer per 100,000 women. This will be possible if they achieve the WHO 90-70-90 targets by 2030 (illustrated to the left).
Achieving these targets in low and middle-income countries (LMICs) alone will prevent 300,000 deaths by 2030 and 14 million deaths by 2070. The 90-70-90 targets may sound ambitious, but we know the technology and tools exist. The WHO Global Action Plans for the Prevention and Control of Non-Communicable Diseases (NCDs) 2013-2030 identifies Human Papilloma Virus (HPV) vaccination, cervical cancer screening, and treatment as cost-effective ‘best buys’.
The evidence is there; now the question remains, ‘is there sufficient political will, multi-sectoral collaboration, support for universal health coverage, and resource mobilisation to make this a reality for ALL girls and womxn by 2030?’
HPV vaccination of adolescent girls before they become sexually active is the most cost-effective, long-term intervention for reducing the risk of cervical cancer. Countries such as Rwanda exemplify what can be achieved by scaling up HPV vaccination and screening services. Since the introduction of the HPV vaccination program in 2011 and screening in 2013, cervical cancer incidence and mortality have declined by 5% and 7.5%, respectively, amongst Rwandan girls & womxn. In the UK, HPV vaccination has led to an 87% decrease in cervical cancer in England between 2008 and 2021. Given the long gap between HPV infection and the development of cervical cancer, significant declines in cervical cancer in Rwanda, similar to England, will be seen in future decades.
Some girls and womxn will miss or are ineligible for HPV vaccination. Despite increased efforts to scale-up HPV vaccination and screening, over half a million womxn globally will develop invasive cervical cancer in the next two decades.
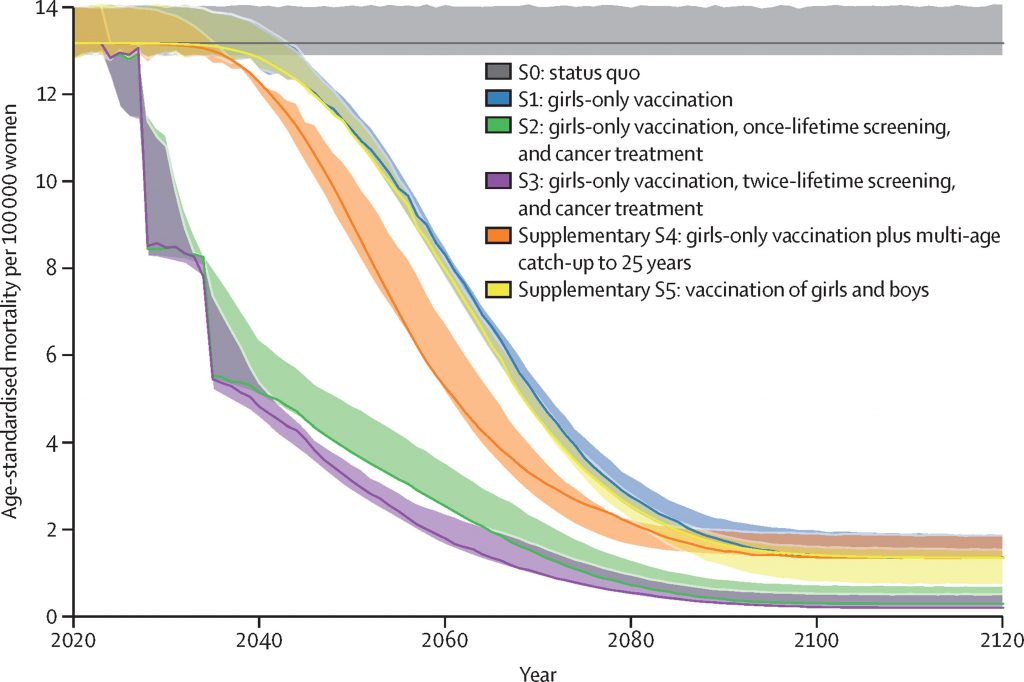
As illustrated to the right, studies reveal that cervical cancer deaths can be reduced from 14 to 2 per 100,000 years within 20 to 40 years compared to 80 to 100 years if countries invest in cancer treatment alongside vaccination of girls and twice lifetime screening (S3), compared to the status quo of no vaccination, screening or cancer treatment (S0) or girls only vaccination (S1). Therefore substantial scale-up of cervical cancer treatment is will significantly contribute to the sustainable development Goal (SDG) of reducing NCD premature deaths by a third in 2030.
For decades, cervical cancer management has been ignored or deprioritized because of perceptions of high cost and implementation challenges. This is not accurate.
Dr Bente Mikklesen, WHO Director, Department of Noncommunicable Diseases Tweet
Surgical conditions, including cervical cancer, account for a third of the global burden of disease (greater than malaria, TB and HIV combined). Yet 5 billion people lack access to safe, timely, and affordable surgery. Surgical and or Radiotherapy treatment of early-stage cervical cancer are curative and or life-prolonging, but are still perceived as too difficult, too complex, and too expensive. In countries where there is timely access to high quality treatment, more than 8 out of 10 womxn will survive well beyond 5 years from diagnosis.
Currently, the majority of womxn diagnosed with cervical cancer in LMICs present late with advanced disease that requires curative radiotherapy and of chemotherapy, as well as access to palliative care.
Global disparities stand in our way to achieving cervical cancer elimination. Over 90% of high-income countries(HICs) in comparison to 40% of LMICs have access to cervical cancer treatment and management services. In the USA, minoritised womxn and womxn living in rural areas have less access gynaeoncology services. In the UK Black womxn are overrepresented in the excess morbidity and mortality statistics for cervical cancer. Does the recently reported 87% decline in cervical cancer numbers apply to them as well?

As screening becomes more widespread and accessible, the number of diagnoses of early cervical cancer will increase whilst HPV vaccination is being scaled up more equitably worldwide. These womxn will need treatment, including surgery, radio-chemotherapy, and palliative care.
Investing in strengthening health systems to provide high-quality surgical care contributes to reducing premature deaths and disability, thus increasing the economic productivity and wellbeing of individuals, communities, and nations.
To leave no one behind we must upscale surgical care for cervical cancer
Global Surgery Foundation Tweet
Investing in surgery goes beyond the surgeon’s scalpel and specific surgical procedures. Access to cervical cancer surgery encompasses the entire health care ecosystem required to provide high-quality surgical care and comprehensive cancer control. The roots and branches of this ecosystem bridge primary, secondary, and tertiary prevention & control. “Surgery” includes robust referral networks, functional information & technology (IT) systems, effective governance, sustainable funding, continuous training, recruitment, and retention of specialised workforce including surgeons, anaesthetists, and palliative care nurses, as well as supportive infrastructural considerations like medical supply chains, blood banks, pathology, and nuclear medicine services.
Essentially, surgical systems strengthening is health systems strengthening. Strong surgical systems which effectively treat and manage womxn with cervical cancer will also provide safe, timely caesarean sections for mothers in obstructed labour, functional blood banks to support the closure of open fractures following a road traffic accident, as well as anaesthetic and nursing expertise for patients undergoing laparotomy(open surgery). Investing in improving IT systems, transport, and referral networks that promptly connect womxn to cervical cancer management options including chemo-radiotherapy, palliative care, and surgery will also benefit individuals who try to access care when diagnosed with other types of cancers.

At the recent World Health Summit, Dr. Cherian Varghese, WHO lead for NCDs and special initiatives stated that “…Surgery is a great unifier“. I agree with him.
Womxn, girls, and families diagnosed with cervical cancer can no longer afford for “Surgery” to be the neglected stepchild of cervical cancer control.
It is our aunties, mothers, sisters, neighbours and best friends that die of cervical cancer. The question is no longer can we save them, it is, will we invest in saving their lives?
Isioma Okolo Tweet
In my pieces, I use the terms:
Girls, women, womxn, pregnant people and birthing people to refer to some of the reproductive health experiences of individuals assigned female at birth. Not all women have cervixes, not all people who have cervixes identity as women.
Minoritised in place of BIPOC( Black, Indigenous & people of color), POC ( people of color), BAME (Black, Asian & Minority Ethnic) and BME ( Black & Minority Ethnic) to recognise that individuals and communities do not naturally exist as minorities; but instead have been assigned this identity in response to dominant socio-economic and political narratives. ‘Minoritised’ intentionally highlights contemporary power imbalances rooted in historical events of slavery, colonisation, and other systems of oppression
The Economics of Your Uterus, dissecting out why your anatomy pre-determines your tax bracket and chances of becoming a millionaire
Sullivan R, Alatise OI, Anderson BO, et al. Global cancer surgery: delivering safe, affordable, and timely cancer surgery. Lancet Oncol. 2015;16(11):1193-1224. doi:10.1016/S1470-2045(15)00223-5
Meara JG, Leather AJM, Hagander L, et al. Global Surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Surgery. 2015;158(1):3-6. doi:10.1016/j.surg.2015.04.011
The menopause is a natural part of the female life cycle. But why do women become invisible after the menopause? Dr Jen Gunter answers my question 'Ain't I A Woman?"
The menopause is a natural part of the female life cycle. But why do women become invisible after the menopause? Dr Naghat ARif answers my question " Ain't I A Woman?"
In this game of gonads, who decided that a testicle is worth more than an ovary?
To deputise a complete stranger to interfere with a woman’s health choice is constitutionally, medically, morally and ethically wrong. That's the end of my sentence.
Cervical cancer can be prevented. When detected early it can be treated and cured with surgery. As we mark the one year anniversary of the "Cervical Cancer Elimination Day of Action", I reflect on the role of surgical systems in eliminating cervical cancer.
Adolescents make up 16% of the population and straddle the sometimes uncomfortable gap between childhood and adulthood. Seeking out information on the internet makes sense but at what cost?
Periods don't have to cost us education, equity and the environment
We had no say in the decision of when, how, where and to whom we were born. Yet this was one of the most important decisions in our lives, which continues to impact us today.
More from Isioma Dianne Okolo here.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.