Aina M, Igbokwe U, Ibrahim R, Aladeshawe S, Mmrikwe I, Jegede O, Ajuwon I, and Aigbogun E. The role of leadership and management capacity building in driving institutional transformation in public sector organizations: a case study of National Primary Health Care Development Agency – Leadership Development Academy. HPHR. 2024;87.
The National Primary Health Care Development Agency (NPHCDA) in Nigeria created the Leadership Development Academy (LDA) in 2018 to improve staff skills for better healthcare delivery. This program has significantly enhanced the agency’s ability to provide technical assistance (TA) and improve healthcare access and quality nationwide.
This paper explores the pivotal role of leadership and management capacity building in driving substantial institutional transformation within public sector organizations using the National Primary Health Care Development Agency (NPHCDA) Leadership Development Academy (LDA).
This study was an evaluation report of the capacity building initiatives of the NPHCDA LDA, the successes achieved by the enrollees of the LDA, their assigned roles following the capacity building intervention, and the resulting impact.
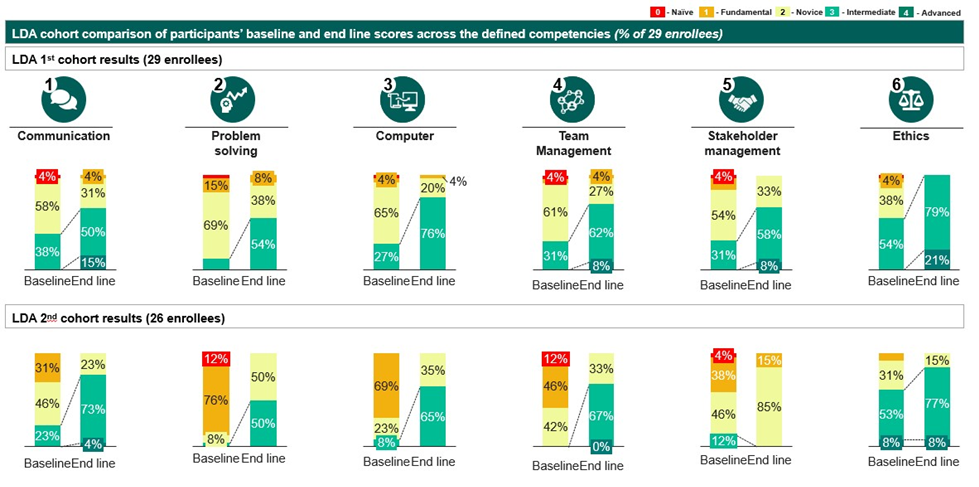
Between 2019 and 2020, the LDA graduated two cohorts of 29 and 27 fellows, with 41% and 57% acquiring intermediate to advanced competencies, respectively. These skilled TA providers subsequently led key initiatives such as subnational intervention coordination, the National Ward Health System Strategy, the 2020 integrated medical outreach program, and the COVID-19 vaccine rollout, which reached over 130 million citizens.
The capacity building approach by NPHCDA LDA demonstrates how effective leadership and management capacity building equip leaders with essential skills to inspire vision, foster innovation, and ensure accountability, driving substantial improvements in service quality and organizational success. The program’s success highlights the crucial role of adaptive leadership and management capacity building in enabling public sector organizations to effectively tackle challenges, foster innovation, and adapt to evolving demands. The NPHCDA case study serves as a compelling example of how leadership development initiatives can have cascading positive effects on various aspects of public sector operations.
Public sector leaders can learn from NPHCDA’s approach by identifying capacity gaps, implementing tailored capacity building, and continuously evaluating outcomes. This case highlights how leadership development can significantly enhance service quality and drive broader societal advancement.
Public sector organizations are tasked with addressing the multifaceted needs of society, ranging from healthcare and education to infrastructure and governance.1,2 Their capacity to deliver services efficiently, allocate resources judiciously, and adapt to an ever-evolving environment directly reflects the leadership and management competencies of its workforce. Effective leadership instills vision, fosters innovation, and imparts accountability,3 while adept management optimizes resource allocation, streamlines operations, and enhances service quality.4,5 Training and development help to ensure that organizational members possess the knowledge and skills they need to perform their jobs effectively, take on new responsibilities, and adapt to changing conditions.6
Many public sector organizations in low-middle income countries struggle to translate leadership and management capacity building into organizational transformation because (i) the focus of the capacity development is rarely tailored to the skills the organizations need;7 (ii) capacity building approaches are more mainstream and not contextualized to the realities within the organizations,8 and (iii) skills learned are not applied, as trainees find it difficult to translate skill gained from capacity building into job execution. 7 Though there are a number of factors, such as financial resources, human resources, and infrastructure, which collectively contribute to organizational transformation, human resources stand out as the most significant factor among them.6
Such training is essential for advancing social justice and health equity, as it empowers leaders with a transformative mindset to advocate effectively for social conditions and physical environments which promotes inclusivity.9 By equipping them with strategic, culturally competent skills, these leaders are better positioned to drive inclusive policies and promote equitable access to healthcare, thereby addressing the needs of underserved populations and fostering systemic change.3,9
The National Primary Health Care Agency (NPHCDA) aims to develop and promote primary health care, control preventable diseases, and improve access to quality health services in Nigeria.10 This mission involves coordinating all PHC services nationally and at the national and subnational level through the thirty-six State Primary Health Care Management Boards (SPHCMBs). However, achieving this mandate necessitated a critical resource: technically skilled staff with management competencies to effectively deliver transformational initiatives of primary health care (PHC). Recognizing this need, the Agency had previously deployed a few capacity building interventions to bridge this gap, which had not yielded the desirable and sustainable results.11,12
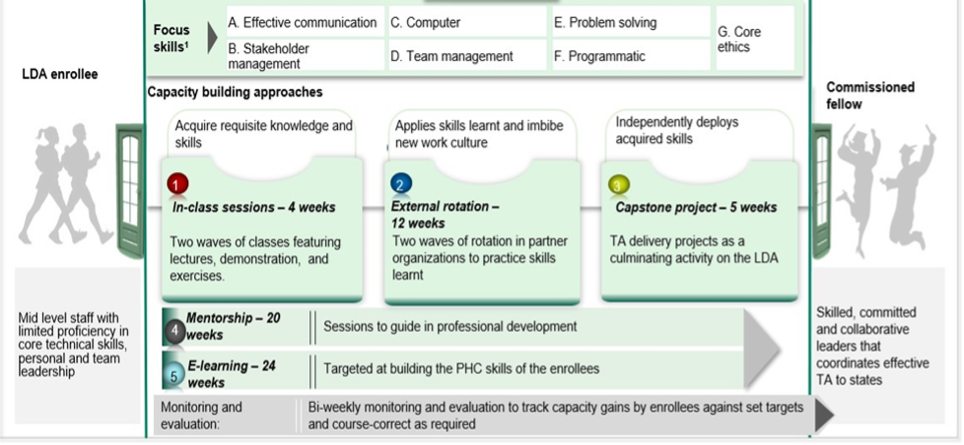
Considering the common pitfalls in designing and implementing capacity-building programs in public sector institutions of low-income countries (LICs), the Agency aimed to create a program to drive institutional transformation and achieve its organizational mandate. The Leadership Development Academy (LDA) was established to enhance the capacity of technical staff, enabling them to effectively coordinate and provide technical assistance as TA providers, and act as change agents driving institutional transformation at both the Agency and sub-national levels.13 This study examines how leadership and management capacity building at the NPHCDA Leadership Development Academy drives impactful institutional change, showcasing it as a practical model for public sector organizations.
This study conducted an in-depth evaluation of the capacity-building initiatives of the National Primary Health Care Development Agency (NPHCDA) Leadership Development Academy (LDA). The methodology comprised several key components:
The Agency designed the LDA with technical support from the Solina Centre for International Development and Research (SCIDaR) and Bill & Melinda Gates Foundation (BMGF) funding. The design of the LDA involved several iterative sessions between the NPHCDA leaders and mid-level staff to identify the gaps and the best approaches to bridge them. The NPHCDA developed a capacity building framework (Figure 1) to efficiently deploy a tailored capacity building program to address its staff’s leadership and management competencies.
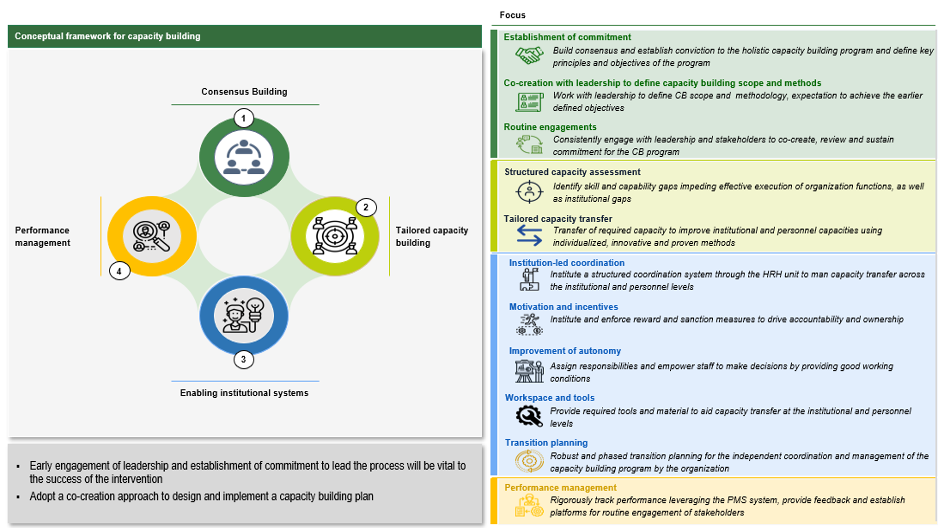
The capacity building framework builds on four core pillars to foster and maintain staff capacity with the overall aim of driving organizational transformation as follows:
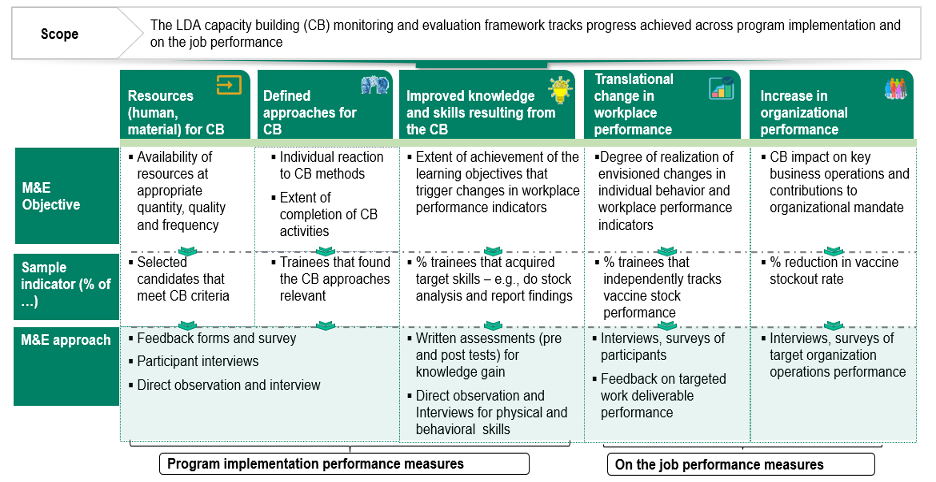
The role of leadership and management capacity building in driving institutional transformation within public sector organizations, as exemplified by the National Primary Health Care Development Agency (NPHCDA) Leadership Development Academy (LDA), is described in Figure 4 – 8. This approach proved to be very effective in catalyzing the Agency’s transformational process from the baseline in 2019 to the end of the capacity building program in 2020.
Between 2019 and 2020, the LDA graduated two cohorts of 29 and 27 fellows. About 41% and 57% of enrollees acquired intermediate to advanced competencies between the baseline and end-line assessment in the first and second cohorts, respectively (Figure 4). The LDA fellows took up more challenging roles like leading teams and work streams such as TA intervention coordination at the sub-national level, Development of the National Ward Health System Strategy, the 2020 integrated medical outreach program to catch up from the impact of the pandemic, and the successful introduction of the COVID-19 vaccine into Nigeria, which has reached over 130 million citizens.7
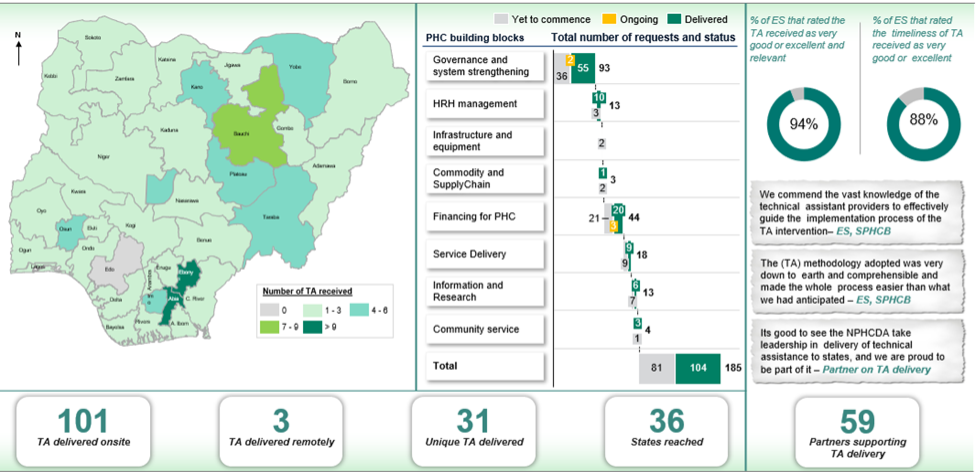
Through the LDA program, the Agency has instituted a Technical Support Unit (TSU) that coordinates the deployment of resources to fulfill the Technical Assistance gap across the country. The TSU functions with over 30 TA providers (fellows of the LDA program) equipped with the pre-requisite leadership and management competencies to support SPHCBs in achieving their organizational mandate. The TA providers are responsible for providing technical resources to fulfill TA gaps at the subnational levels.
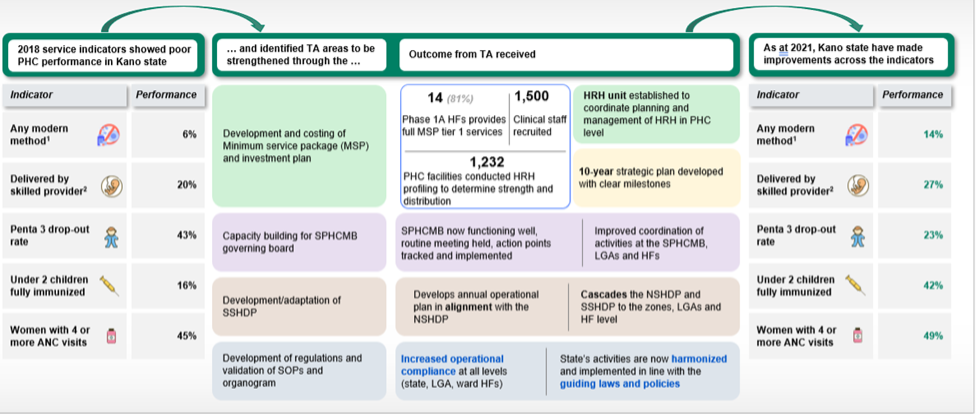
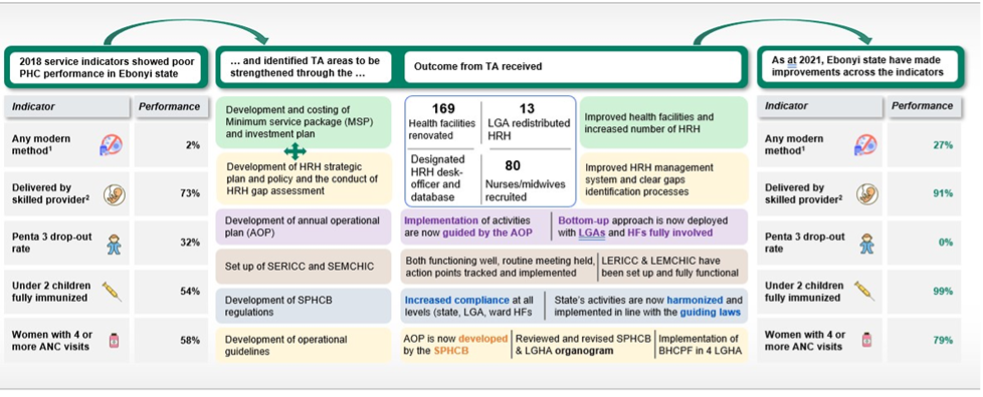
A total of 101 (31 unique) Technical Assistance requests from the sub-national entities have been fulfilled by this cohort of fellows with support areas (Figure 5) ranging from Annual Operational Plan (AOP) development, Minimum Service Package (MSP) development and Investment planning; Capacity building for State Primary Health Care Management Board (SPHCMB) governing board, etc. So far, 36 SPHCMBs across all six geopolitical zones of the country have benefitted from this initiative through several approaches, strengthening the National agency’s responsiveness to the states’ needs and optimizing the country’s overall Primary Health Care system.
Equipping the NPHCDA staff with the required competencies through the LDA bolstered the Agency’s ability to execute activities that typically would require support from external consultants, saving significant financial resources for the Agency and its partners. The LDA results continue to fuel the vision of the Executive Director of NPHCDA to drive work culture transformation at NPHCDA by building a critical mass of competent and dedicated staff.
Capacity building plays a crucial role in developing effective leadership by equipping leaders with the skills and knowledge necessary to inspire a clear vision, foster innovation, and promote accountability.3,4,17 Through targeted training programs, the NPHCDA leaders learned how to inspire and guide their teams using effective communication strategies to achieve the organizational objectives. Building capacity helps leaders think creatively and solve problems, which makes it possible for them to be agile in a dynamic organizational environment and operating ecosystem.4,18 Additionally, it instills a sense of responsibility and ethical conduct, ensuring leaders hold themselves and their teams accountable for their actions and results, eventually promoting organizational success and sustainability.19
The Agency implemented a thoughtful approach to ensure that the NPHCDA could enhance the quality of PHC services and improve access nationally and at the subnational level. Following a defined selection criterion, the LDA’s reach was purposely spread across the geopolitical zones to ensure equitable availability and distribution of technical resources at the subnational level. Moreover, to effectively impact change at the state level, the Agency established robust mechanisms to address state-specific needs targeted at transforming PHC delivery. This included designing and institutionalizing a dedicated platform for State Primary Health Care Management Boards (SPHCMBs) to identify TA gaps across the various PHC building blocks. This mechanism triggered many activities, leading to the deployment of the LDA fellows’ skilled TA providers to address these gaps. This approach was instrumental in ensuring the availability of skilled personnel at the subnational level and significantly improving the quality of services across the PHC building blocks.
The Agency’s experience with the LDA program, including both cohorts, has been exceptionally positive. The competencies demonstrated by LDA fellows have led to program adaptations, such as developing a new-hire training program to train and ease the transitioning of new hires into the Agency and routine capacity-building interventions for program officers of the Program Implementation Unit (PIU) and departments. Additionally, the learning modules from the LDA have been leveraged to create the NPHCDA e-learning platform, extending the program’s reach and impact across the Agency. The NPHCDA e-learning platform was developed in response to positive feedback from fellows who found the courses valuable for their work at the Agency. To extend these benefits and address the high costs of physically training all staff, the platform was established as a more accessible alternative. The initial rollout involved the fellows, who provided feedback that informed further improvements. Consequently, the e-learning platform became an integral part of the Agency’s continuous improvement plan, ensuring that all staff could benefit from ongoing training and development. Beyond the professional growth experienced by LDA fellows and the evident successes at the subnational level, the LDA program has also fostered a culture of continuous learning and development within the Agency.
Training programs such as the LDA capacity building for leaders equip them with the skills needed to excel in their roles, thereby improving the organization’s operational systems. According to the American Society for Training and Development (ASTD), organizations that invest heavily in employee training and development see a 24% increased performance than those that spend less on training.20 This is because well-trained employees are more efficient, make fewer errors, and require less supervision, increasing productivity.20-22
The NPHCDA’s Leadership Development Academy (LDA) illustrates how strategic capacity building can drive transformative change in public sector organizations. The findings from this program emphasize that tailored capacity building, practical learning approaches, motivation enhancement, and robust monitoring and evaluation are critical success factors in achieving transformative change. Public sector leaders can learn from NPHCDA’s approach by identifying capacity gaps, implementing tailored capacity building, and continuously evaluating outcomes. This case highlights how leadership development can significantly enhance service quality and drive broader societal advancement.
This study in-depth evaluation of the National Primary Health Care Development Agency (NPHCDA) Leadership Development Academy (LDA) is thorough but there are some limitations. First, the use of a process evaluation and pre- and post-assessments primarily focuses on immediate outcomes, potentially unable to account for long-term impacts of the program on participants and the organization long term goal of advancing health equity. Additionally, while the role assignment and impact evaluation provide insights into the contributions of LDA graduates, the study be able to account for external factors influencing these outcomes, such as changes in the broader health system environment. The study’s reliance on self-reported data from participants could introduce bias, as participants may overstate their improvements or downplay challenges. Finally, the study is context-specific, focused on the NPHCDA, which may limit the generalizability of its findings to other settings or organizations with different structures and challenges.
The authors would like to express their gratitude for the generous support from the Bill and Melinda Gates Foundation, which provided the necessary funding to pilot this innovative initiative. Additionally, heartfelt appreciation goes to the National Primary Health Care Development Agency (NPHCDA) for their unwavering enthusiasm and leadership in conceptualizing and executing this unique approach to capacity building.
This study did not require ethical approval as the pre-and post-assessment focused solely on describing the program’s success rather than evaluating individual participants. The assessment was anonymized, with no physical contact or collection of personally identifiable information involved.
The author(s) declared no potential conflicts of interest concerning this article’s research, authorship, and/or publication.
The author(s) disclosed receipt of the following financial support for this article’s research, authorship, and/or publication: This research was funded by the Bill and Melinda Gates Foundation (Grant No. INV-009819/AMD-10).
Muyi Aina is a seasoned management consultant and public health professional with several years’ experience in healthcare and management consulting. Muyi received his medical degree from University of Ilorin in Nigeria, and holds an MPH in International Health from Harvard University and a PhD in infectious disease epidemiology from Johns Hopkins Bloomberg School of Public Health. He also earned a certificate in vaccine science and policy from Johns Hopkins University.
Dr. Uchenna Igbokwe is the Executive Director and Chief Executive Officer (ED/CEO) at SCIDaR with over 13 years of experience designing and implementing health systems strengthening interventions to improve health outcomes across Africa. He obtained an MSc in International Health Management from Imperial College Business School, London, and Bachelors of Medicine and Surgery from Obafemi Awolowo University, Nigeria.
Dr. Raihanah Ibrahim is a public health, gender and development professional with extensive experience in innovation and strategy, program design, implementation, and monitoring, as well as organizational strengthening and capacity building. She holds a Bachelor of Medicine and Surgery from Ahmadu Bello University, Nigeria.
Dr. Shina Aladeshawe is a Senior Program Office, Global Development at Bill & Melinda Gates Foundation. Shina has over 10 years’ experience in strengthening vaccine supply chain management, malaria interventions, and human resource for health portfolios in Nigeria. He holds an MBChB from Obafemi Awolowo University, Ile Ife, Nigeria.
Pharmacist Ijeoma Mmrikwe is a Senior Associate at SCIDaR, with over 5 years’ experience in health system strengthening and malaria programming. She received her formal training in Pharmacy (Bachelor of Pharmacy) from the University of Nigeria.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.