Ahmed Ali D, Ahmed Ali I, Maheshwari C. The use of hyperbaric oxygen therapy in the treatment of diabetic retinopathy; A systemic review. HPHR. 2022;67.
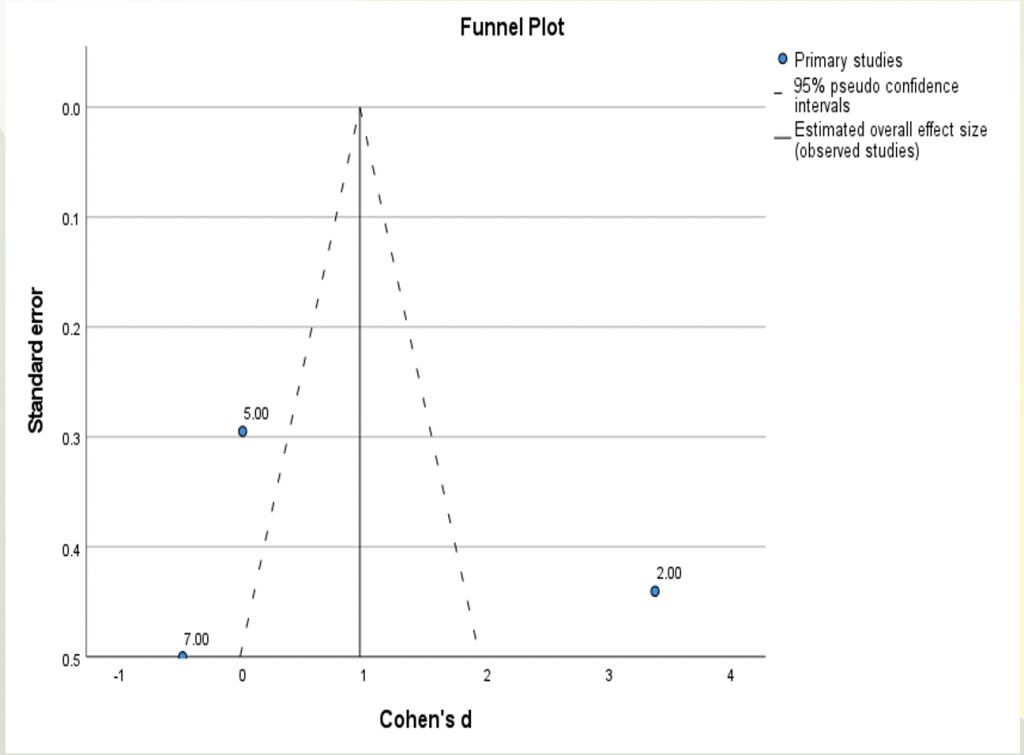
A total of 8 studies were selected. All studies involved diabetic human participants, Aged greater than 18, having diabetic retinopathy, having diabetic foot ulcers except Chang et al study which involved animal participants (male rats) in which diabetes was induced through streptozotocin.
Maalej et al [6] and Chang et al [7] , Feng X et al [11], Freilich DB et al [13] showed Hyperbaric oxygen therapy was effective in the treatment of diabetic retinopathy hence diabetic retinopathy showed regression while Sellman et al [8], Kaldırım H et al [9], Kaldırım H et al [10] showed that hyperbaric oxygen therapy was not effective in the treatment of diabetic retinopathy and diabetic retinopathy neither showed progression nor showed regression. Okamoto N et al [12] showed hyperbaric oxygen therapy can increase the progression of diabetic retinopathy.
Some studies showed the effect of hyperbaric oxygen therapy on the macula. Maalej et al showed hyperbaric oxygen therapy improves diabetic macular edema [6] while Sellman et al [8] and Kaldırım et al [9] showed hyperbaric oxygen therapy induces macular edema or thickens the macula respectively.
Chang et al also observed hyperbaric oxygen therapy was successfully diminishing the extent of the increased blood-retinal barrier breakdown.
Related to the relation of other ocular complications with HBOT, Kaldırım H, et al [10] showed that HBOT increases IOP in type 2 diabetic patients. Feng X et al [11] showed HBOT improves branch retinal artery occlusion along with diabetic retinopathy. Okamoto N [12] showed hyperbaric oxygen therapy increases blood velocity by 20.6 +/- 9.5% in diabetic patients.
HBOT as a treatment option has been indicated in many conditions like diabetic foot ulcers. [14] The use of HBOT in the treatment of diabetic retinopathy is still controversial and the exact mechanism is still unknown. The HBOT causes hyperoxia which causes vasoconstriction, hence which can lead to a decrease in macular edema shown by Maalej et al. HBOT also reduces the expression of pro-inflammatory cytokines, resulting in reducing inflammation [15-17] and increasing oxygen content in the tissue [18] hence this can lead to the healing of diabetic retinopathy. Kaldırım H et al stated that HBOT leads to angiogenesis and cause new vessels to form which in turn increase oxygen content in hypoxic tissue and help to heal diabetic retinopathy. [10]
Regarding the mechanism of action behind the effective use of HBOT in the treatment of diabetic retinopathy is stated by Dumitru R et al which says that HBOT increases blood concentration of the oxygen, which becomes sufficient for tissular needs. This makes possible the survival of some tissues insufficiently supplied with blood. Hence HBOT can be indicated in diabetic retinopathy, retinal venous obstruction, and hypertensive retinopathy. [19]
The mechanism of action behind HBOT causing diabetic retinopathy is stated by McMonnies CW et al who conducted a systemic review regarding the ocular complications due to HBOT and states that HBOT increases oxygen pressure and concentration of reactive oxygen species in blood and tissues which can lead to cataract, diabetic retinopathy, and keratoconus [20]
As compared to the systemic review conducted by McMonnies CW et al in 2015 states that HBOT causes ocular complications like diabetic retinopathy [20] but this systemic review shows that the majority of the studies are in favor of the usage of HBOT in the treatment of diabetic retinopathy [6,7,11,13] and shows effective and positive findings while only one study conducted by Okamoto N et al [12] showed HBOT leads to diabetic retinopathy while others show HBOT neither progress nor regress diabetic retinopathy[8-10]
Studies regarding the harmful effect of hyperbaric oxygen therapy on the retina are rare. One observational study showed that the progression of non-proliferative diabetic retinopathy to proliferative diabetic retinopathy due to hyperbaric oxygen therapy is rare. [21]
A brief literature search on this topic “The harmful effect of hyperbaric oxygen therapy on the retina” showed no cases. In a double-blind, randomized trial (meeting abstract only) of 15 diabetic patients with both NPDR and PDR, patients in neither the HBOT (243 kPa for 90 min) nor the control arm had evidence of neovascularization nor worsening of their proliferative retinopathy at three-month follow-up. [21]
HBOT is considered the safest medical treatment and side effects are rare [22] including barotrauma which occurs in 2% of treated patients and can be prevented by auto inflation techniques or inserting tympanostomy.[22] Another complaint is claustrophobia which requires reassurance and coaching. Oxygen toxicity in the lungs and myopia are infrequent and reversible after stopping HBOT [22].
The majority of studies included in the systemic review showed that HBOT is effective in the treatment of diabetic retinopathy but still some studies oppose it. Hence the use of HBOT in the treatment of diabetic retinopathy is still controversial. Further studies are needed in this regard.
Stoekenbroek RM, Santema TB, Legemate DA, Ubbink DT, van den Brink A, Koelemay MJ. Hyperbaric oxygen for the treatment of diabetic foot ulcers: a systematic review. Eur J Vasc Endovasc Sur 3. Barnes RC. Point: hyperbaric oxygen is beneficial for diabetic foot wounds. Clin Infect Dis 2006. Jul;43(2):188-192. 10.1086/505207 [PubMed] [CrossRef] [Google Scholar]
. Barnes RC. Point: hyperbaric oxygen is beneficial for diabetic foot wounds. Clin Infect Dis 2006. Jul;43(2):188-192. 10.1086/505207 [PubMed] [CrossRef] [Google Scholar]
Cianci P. Advances in the treatment of the diabetic foot: Is there a role for adjunctive hyperbaric oxygen therapy? Wound Repair Regen 2004. Jan-Feb;12(1):2-10. 10.1111/j.1067-1927.2004.012104.x [PubMed] [CrossRef] [Google Scholar]
. Niinikoski JH. Clinical hyperbaric oxygen therapy, wound perfusion, and transcutaneous oximetry. World J Surg 2004. Mar;28(3):307-311. 10.1007/s00268-003-7401-1 [PubMed] [CrossRef] [Google Scholar]
. Barnes RC. Point: hyperbaric oxygen is beneficial for diabetic foot wounds. Clin Infect Dis 2006. Jul;43(2):188-192. 10.1086/505207 [PubMed] [CrossRef] [Google Scholar] [Ref list]
Dumitru R. Metoda hiperbară în tratamentul retinopatiei diabetice, alternativă a terapiei cu laser? [The hyperbaric method in the treatment of diabetic retinopathy, an alternative to laser therapy?]. Oftalmologia. 1993 Jan-Mar;37(1):12-6. Romanian. PMID: 8507603.
. McMonnies CW. Hyperbaric oxygen therapy and the possibility of ocular complications or contraindications. Clin Exp Optom. 2015 Mar;98(2):122-5. doi: 10.1111/cxo.12203. Epub 2014 Oct 12. PMID: 25308346.
. Tran V, Smart D. Proliferative retinopathy during hyperbaric oxygen treatment. Diving Hyperb Med 2017. Sep;47(3):203. [PMC free article] [PubMed] [Google Scholar] [Ref list]
Chen J. The Effects of Hyperbaric Oxygen Therapy on Diabetic Retinopathy. Invest Ophthalmol Vis Sci 2003. May;44(13):4017-4017. [Google Scholar]
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.