Year-to-Year comparison of Virginia’s Hepatitis education and patient connection referral on release program outcomes for those recently released from incarceration. HPHR. 2022;56.10.54111/0001/DDD1
The purpose of this review is to outline the Virginia Hepatitis Education and Patient Connection. Referral on Release (HEPC-RoR. This program for increasing access to treatment for hepatitis C for those recently released from incarceration, including first-year outcomes, quality improvement practices that were implemented post first year, and second year program data. Using this information, we hope to inform organizations attempting to implement similar programs of potential challenges and corresponding solutions. Alternatively, we hope to share potential program designs for organizations that have identified a need for programs to support linkage to care for those recently released from incarcerated.
After analyzing first-year program data, we identified areas for improvement. Based on these findings, the team implemented new processes. After a review of the second-year data, we found significant improvement in clinical data, program workflow, and data quality from the previous year. A change in workflow allowed us to collect additional correct contact data, connect more patients to care and ultimately to cure their hepatitis C. Our database, which was redesigned following year one, provided formatting changes allowing for expedited data extraction and review. The process between facilities also improved, streamlining efforts and alleviating some strain associated with limited staffing.
Following the review of first-year HEPC-RoR data, program strengths and weaknesses were identified, and a quality improvement plan was developed to addresses areas of need. Changes included more frequent and varied outreach, follow-ups to community partners for confirmation of appointments and lab results, and a redesigned database for more comprehensive data collection. Second-year program data found significant clinical outcomes, such as an 86.7% linkage to care rate and a 23.5% cure rate, and improved referral and database quality.
Hepatitis C virus (HCV) is the most common blood-borne infection in the United States (US). 1 The primary transmission of HCV is through intravenous drug use (IVDU) with unsterile equipment.2 Depending on the medication prescribed, HCV can be cured in 8-12 weeks.3 It is estimated that 30% – 40% of all people infected with HCV in the US pass through the correctional system annually.4 Approximately 33% of incarcerated individuals in the United States had HCV in 2013.5 In Virginia in 2019, there were 36,091 prisoners under the jurisdiction of state or federal correctional authorities, and 31,838 in 2020.6 Virginia, as most states in the US, has not historically kept track of the incidence of HCV within the prison system.7 Treatment for HCV among the incarcerated population has remained limited due to availability of resources or treatment parameters.8
The need for increased access to treatment for HCV is statewide in Virginia. This need led to a partnership between the Virginia Department of Health (VDH) and the University of Virginia (UVA) to create the Virginia Hepatitis C Education and Patient Connection (HEPC) program. The HEPC program aims is to expand access to HCV treatment to heavily impacted communities. The program began doing this by offering telemedicine visits with a UVA Infectious Disease specialist to rural areas in Southwest Virginia. The HEPC program then expanded to offer a training program for community providers and their support staff to learn to treat hepatitis C among their patients locally. This training was implemented after the Virginia Department of Medical Assistance Services removed the requirement for specialty providers to treat HCV in 2018 and included education about the disease process, medications to treat, patient perspectives, epidemiology and harm reduction. The training ensured the providers were up to date on treatment protocols which included the removal of sobriety requirements for patients to begin treatment in 2019 by the American Association for the Study of Liver Diseases (AASLD), and the removal of the prior authorization requirement by Virginia Department of Medicaid in January 2020.9 After completion of the training, participants were able to treat independently, navigate patients through the treatment process, maintain access with the UVA Infectious Disease medical provider for consultation on any patient, and participate in monthly case study webinars to continue to grow their knowledge of HCV.10
Recognizing that the incarcerated population represented a significant portion of HCV infections and the need for concentrated policy and clinical work that would increase capacity for treatment within this population, the Virginia Department of Corrections (VADOC) began working with the HEPC program with aims to increase treatment options. Pharmacists from VADOC were among some of the first providers to attend the HEPC training program. The pharmacists immediately began to implement treatment within VADOC. However, barriers that prevented HCV treatment while incarcerated remained, and many people were released from incarceration with active HCV infection.11
In Virginia, barriers included restrictions related to the degree of scarring (fibrosis) of the liver, amount of time left on the person’s sentence, and the facility housing the incarcerated individuals, as not all of them had 24 hour nursing care.12
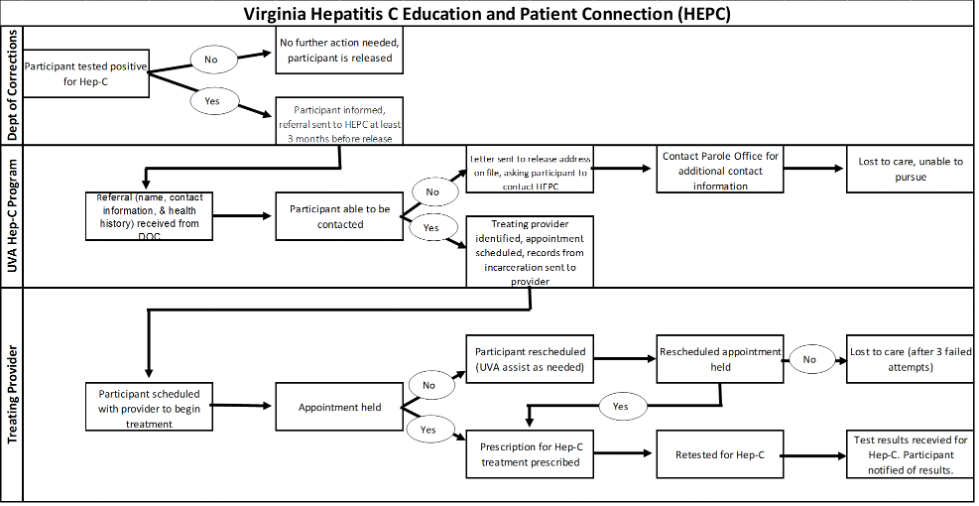
The partnership between VADOC and Virginia HEPC facilitated the creation of a program to provide navigation to care for those released with untreated HCV to increase access to treatment upon their release. This program is known as the HEPC- Referral on Release (HEPC-RoR) program. To meet this goal, the HEPC-RoR program pulled from the foundational work and network of the HEPC provider training program to link individuals recently released from incarceration to community providers for treatment. A cross-functional logic model depicts the workflow of task, by agency, to link the participant to treatment (Figure 1).
Figure 1: Cross-functional flow chart of the HEPC RoR program
Within the first year of the program, from August 1, 2019, through July 31, 2020, 638 referrals had been received by the HEPC-RoR program. This amount exceeded what was anticipated by the staff and overwhelmed staffing capacity at the time. Noting that there was high volume and low staffing, the program conducted a review of its data and processes to maximize efficiency. Following the review, changes were made to the program and improved data capture process. At the end of the second year of the program, July 31, 2021, a second review was conducted to see what impact the changes had on clinical outcomes and data capture processes. This review article will focus on the findings from the first and second year reviews, the changes made between the years, and the clinical and workflow outcomes that resulted from those changes.
Data from the HECP-RoR program is stored in an Excel workbook. For this analysis, copies of the active workbooks were made and the data reviewed. Patients who had been incarcerated during their treatment and then re-released following a second incarceration are only counted once in the results.
The first and second-year program reviews were conducted systematically using descriptive statistics in an Excel database. Data collected and reviewed included: the number of referrals received, demographic data, anticipated release date, contact information, labs and diagnostic reports, preferred contact method, linkage to care, progress through the steps to cure, and clinical outcome.
The individual’s progression through the Cascade of Care at the end of the first year included several options: referral received, released, unable to contact, released out of state, re-incarcerated, no viral load, appointment scheduled, started medication, and cured.
To understand the differences between the first-year and second-year data collection process the review primarily focused on the actual data content: the uniformity of collection, the definition of steps in the process, and the ability to tell how individuals were progressing through the HEPC Cascade of Care, and where there were gaps in data.
Once the data was analyzed, using descriptive statics, a year to year comparison was conducted with rate and percentage change calculated.
Of the 638 referrals, 632 (99.1%) of those referred were released from incarceration during year one. Of the 632 released during year one, 57 did not have a detectable HCV viral load upon release, indicating no active infection and no need for treatment. Another 55 of the received referrals were released to out of state addresses; this also excluded them from participation with the HEPC-RoR program. That said, those released to out of state addresses were given education and contact information for national resources. Another 198 of those referred did not have contact information provided or had inaccurate contact information. Ten of the remaining referred persons were re-incarcerated and, therefore, not able to receive services through HEPC-RoR. This left 312 eligible referrals to be contacted.
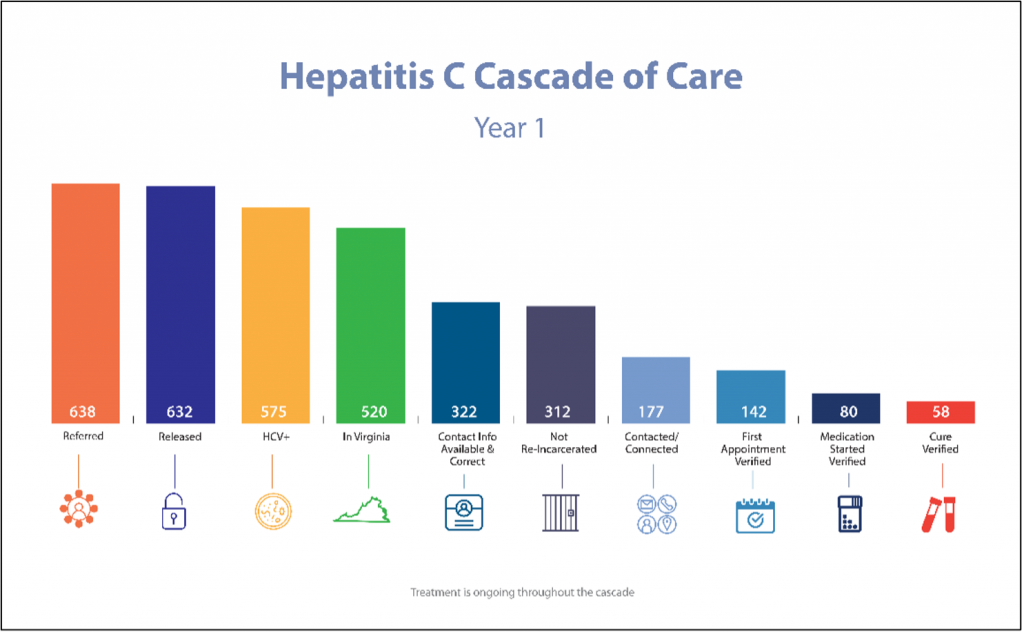
Of the 312, 177 (56.7%) were able to be contacted and connected to care. Of the 177, 142 (80.2%) attended their first appointment for HCV treatment. We were able to confirm that medication was started on 80 (56.3%) of those who attended their first appointment. Of those who started medication for their HCV infection, 58 (72.5%) had a conformational lab test verifying cure of HCV. This succession of participants is referred to as the RoR Hepatitis C Cascade of Care (Image 1).
Image 1: Hepatitis C Cascade of Care for year one of HEPC-RoR program
While there was ample data for review, the clinical dataset required additional curation. For example, common errors such as misspelled words led to data extraction with duplicate fields. In some fields, lab values were reported in their numeric resulted form yet, in the same field the equivalent corresponding alpha value would be listed. For example, a Fibroscan score of 8.1 might be listed for one individual, but have been converted to the Metavir Fibrosis score of F2 for another individual. The need for uniform and structured data fields became apparent, a requirement sometimes overlooked in clinical databases.
There were several fields for which no data had been reported. This was later discovered to be the result of two issues. First, in looking at the source of initial data, referrals from the VADOC, there was little uniformity in how that was received. The VADOC began work on additional education for their staff on appropriate referrals to send and hired a Hepatitis C Coordinator to assist with gathering the demographic, labs, and diagnostic information to send to HEPC-RoR.
Secondly, there was an unanticipated need for continual monitoring of the individuals progression through the Cascade of Care. The HEPC-RoR program began as a referral program, without considering the societal issues facing those recently released when attempting to schedule and travel to appointments with providers. Upon calling to confirm that individuals referred had actually accessed treatment, it was found many of those referred had not attended their scheduled appointment. Calling clinics or referred individuals to see if they had managed to set up an appointment for treatment or if they had attended their already scheduled appointment was not part of the original workflow. However, to ensure access to treatment and cure, while capturing progression and identifying potential barriers, we needed to incorporate outreach throughout the Cascade of Care.
An additional issue was the lack of dedicated staffing to this project. Improving the database capture helped by providing drop down responses which allowed for speedy data input and communication. The addition of a second referral site option field in the database was helpful, as many times the first referral did not work out. HEPC-RoR staff had researched the referral locations to ensure knowledge of what insurances were accepted, any restrictions and any specific requirements for referrals, but barriers persisted. Designated columns to verify location, date of initial visit and drop down responses for reason not linked to care provided needed information to ensure a second referral would be successful. Despite the improvements, the large number of referrals remained overwhelming to staff who added these task to their full-time positions. It became apparent that dedicated staffing to this project would be required.
In the second year of the program, 265 referrals were received, and 263 (99.3%) had been released at the time of this analysis. 2 (0.9%) had been re-incarcerated prior to being contacted by HEPC-RoR and were therefore not eligible for services. Viral load was not detected in 15 of those referred. Another 23 of those referred were being released to an out of state address and were therefore not eligible for services through HEPC-RoR. Contact information was either missing or inaccurate for 69 of those referred. This left a remaining 116 individuals who were eligible for services through HEPC-RoR. Of the 116 who were contacted and connected to care, HEPC-RoR was able to confirm that 112 (96.6%) attended their first appointment for HCV treatment. Of those 112, 96 (85.7%) started medication to treat their HCV. Finally, 11 (11.5%) of those who started medication, have confirmatory lab work known as a sustained viral response (SVR) to show that their HCV has been cured. Currently, 4 (4.2%) of those who started medication are awaiting SVR results. One (1%) of the referred individuals who started and completed medication had a negative SVR test result, indicating treatment failure. Image 2 depicts the Hepatitis C Cascade of Care for year two.
Image 2: Hepatitis C Cascade of Care for year two of HEPC-RoR program
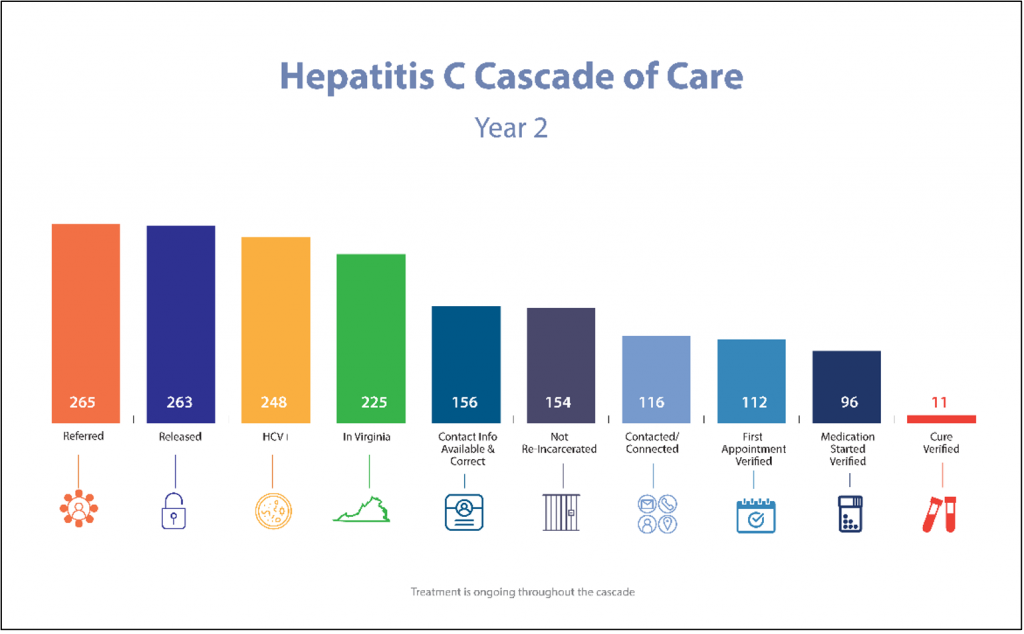
Table 1: Yearly Side-by-side comparison on Steps in the HEPC Cascade of Care
| Year 1 | Year 2 | Years 1 and 2 combined |
Referred | 638 | 265 | 903 |
Released | 632 | 263 | 895 |
HCV+ | 575 | 248 | 823 |
In VA | 520 | 225 | 745 |
Contact info Available and Correct | 322 | 156 | 478 |
Not Re-incarcerated | 312 | 154 | 466 |
Contacted/Connected | 177 | 116 | 293 |
First Appointment Verified | 142 | 112 | 254 |
Medication Started Verified | 80 | 96 | 176 |
Cure Verified | 58 | 11 | 69 |
A year-to-year comparison shows significant differences. There was a dramatic decrease in referrals for year 2. This can be attributed to a few factors. During the first year, we received what were essentially a backlog of patients who needed assistance accessing treatment.
The second factor was the VADOC pharmacists renewed efforts to start treatment within the prison system prior to release. These factors led to a high number of referrals the first year that later tapered off entering the second year of the program. The staffing for Virginia HEPC-RoR did not increase in year two, however the practices of the VADOC on ensuring eligible referrals helped to allow more time for connecting the referrals to care. In year one 112 (17.6%) of the referrals were ineligible for assistance. In year two that dropped to 38 (14.3%). The referrals came with more complete information as well, with contact information being available and correct on 156 (59.3%) of the referrals versus the prior year’s 322 (50.9%) (Table 1)
Our clinical outcomes are still being collected, as referred individuals continue through the steps of the Cascade of Care. When we combined the data from years one and two to understand the broader picture, we see there were 293 eligible referred individuals. 254 (86.7%) of those have attended a first appointment for treatment for their HCV and 69 (23.5%) of those eligible referrals cured of their HCV. Because referred individuals are passing through a cascade of care, or care continuum, these data are rapidly changing. However, we can still ascertain that the program has been meeting its overall goal of linking HCV positive individuals to care, as evident by the 86.7% linkage rate of those eligible, and assisting them to reach cure of their HCV, as evident by the 23.5% cure rate.
The HEPC-RoR program was created and implemented in response to an immediate need to treat those released from incarceration with active HCV infection. Year one data review showed the need for an improved referral process and additional staffing to process the overwhelming number of received referrals. Following a program evaluation at the end of the 1st year, which focused on clinical outcomes, data quality, and workflow, changes were made in an effort to improve outcomes. Much of the improvement plan focused on creating a database with structured fields and coded automation to assist with the tracking of patients through the Hepatitis C Cascade of Care. During this time, funding for dedicated staff was also being discussed among the partners. In addition to the improvement plan, additional experience and training on the side of those referring and those receiving the referrals was being gained as the program continued along with growing recognition by those incarcerated, soon to be released.
During year two of the program, the data quality improvement plan was implemented as was dedicated staff within VADOC to assist with treatment during incarceration. As a result, year two analysis shows significant improvement in clinical outcomes. This is most strongly noted in the number of individuals who started and completed treatment for HCV and the number of individuals who were cured of HCV through the HEPC-RoR program.
Much of this success is due to the workflow changes and the data capture changes. For example, in regards to workflow changes, outreach is now made to the referred individuals following their scheduled appointment to ensure they attended and are progressing towards treatment or to assist with rescheduling if the appointment was not attended. Outreach is also conducted to obtain SVR lab results which indicate if the treatment was successful and the individual is cured of HCV. These outreaches, which were not part of year one workflow, have led to more patients being assisted with navigation to their treatment, data capture and data accuracy. The changes made to the database have led to more robust and fixed, or structured, data which reduces human error and results in cleaner data.
The changes implemented have significantly increased positive outcomes for the program. Most proudly, is the positive impact it has had on the health of those recently released from incarceration in getting treatment, the increased availability of treatment within the VADOC facilities during and after incarceration, and public health at large.
SC and RD provide consulting services that are unrelated to this publication to Warm Health Technology, Inc
We would like to thank VDH, VADOC, and the UVA for their continued partnership and support of the HEPC program. We would also like to thank Patrice Ross, LPN and Devan Kaufman, B.S. for their work and dedication in making this program possible.
Dr. Jamie Smith is the Chief Pharmacist and Clinical Pharmacy Services Manager for the Virginia Department of Corrections and has created and managed a pharmacist-led Hepatitis C (HCV) treatment program offering HCV treatment to patients statewide via telemedicine. Dr. Smith has also coordinated with various state agencies and academic medical facilities to create a referral program for releasing patients to be connected to HCV care, improve HCV screening in facilities statewide, and expand HCV education for incarcerated individuals. Dr. Smith also works to expand clinical pharmacy services within the department and improve patient care by serving on various committees including the Medication Assisted Therapy Taskforce, Opioid Workgroup, P&T committee, Corrections Crisis Intervention Training, and many others.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.