Garg P, Muthiah S, Singla C. Telerehabilitation for COVID-19 patients in India: Problem to Solution. HPHR. 2021; 29.
DOI:10.54111/0001/cc9
COVID-19 has taken a massive toll on the planet, claiming over 3 million lives and infecting nearly 150 million people. (1) This highly contagious multisystem disease is caused by the novel SARS-CoV-2 strain. Originating in Wuhan, China, in December 2019, the infection rapidly pervaded the globe, being declared a public health emergency by the WHO on January 30, 2020, and a pandemic on March 11, 2020. (2)
Despite closely resembling the SARS-CoV-1 and MERS-CoV, the causative agents of two global pandemics in 2003, the SARS-CoV-2 varies widely in the presentation instead of the predicted trajectory. (3) Significant progress has been made in understanding the virus, the infection, and developing treatment protocols. Nevertheless, the long-term effects of COVID remain unknown.
In post-recovery, several heterogeneous manifestations are observed in COVID patients from the acute phase of illness. They vary widely in presentation and are often observed to involve multiple organ systems with consistent, transient, multiple, or fluctuating symptoms. (4) Several terms have been used to denote the long-term effects of COVID 19, including Long COVID, Post-acute sequelae, Post-COVID syndrome, and Post-acute COVID 19. (5) Up to now, a standard clinical definition or the pathogenesis of the Long COVID does not exist. Nor is there a standardized treatment protocol for managing the long-term sequelae of SARS COVID, despite the proactive measures taken by various nations towards preventing and managing the Long COVID, such as the Stanford Hall consensus,(6) the NICE, SIGN, and RCGP guidelines. (7)
Despite being fully treated, COVID-19 patients are still prone to develop persistent dysfunction of almost any organ system and, therefore, develop Long COVID. (8) Thus, rehabilitation, starting at the earliest stage, is needed to help the patients convalesce, especially in developing countries like India.
In early 2021, after what seemed to be a near-complete containment of the transmission, against the backdrop of the biggest vaccination drive, India witnessed a massive rise in the incidence of COVID. It crossed over 800,000 cases in a mere week. India has since seen more than 18 million cases with over 200,000 reported deaths. (9,10) This second wave of COVID in India took the world by surprise, and entertaining the possibility of an impending surge in Long COVID makes the need for proper rehabilitative guidelines all the more critical. Given the circumstances, telerehabilitation will ensure equitable access to rehabilitative care resources for the patients of long COVID.
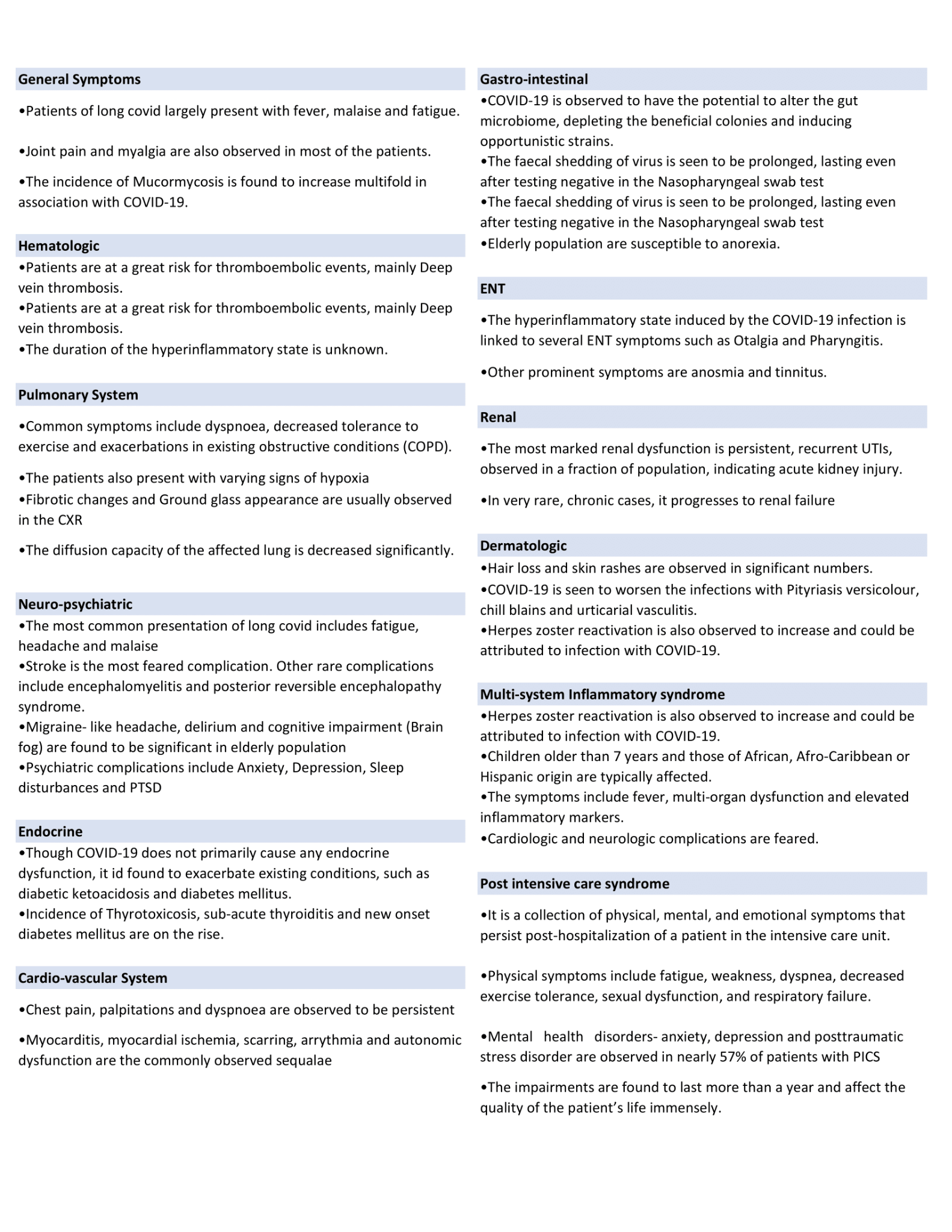
Recorded symptoms of the Long COVID include and do not limit to breathlessness, fatigue, anxiety, depression, cognitive dysfunction, arrhythmias, and myocardial injuries. (11-14) The incidence is seen in all demographic groups. The pediatric population usually has a mild presentation of the acute symptoms of COVID 19. However, the post-acute manifestation showed an increased incidence in the multisystem inflammatory syndrome. (15,16) The incidence of post-intensive care syndrome is also on the rise due to the pandemic. Box 1 lists all the system-wise effects of Long COVID.
Many countries are working toward establishing a protocol for rehabilitating COVID 19 patients and managing the Long COVID. (17-20) Rehabilitation for COVID 19 is being done meticulously, starting right from discharging the patients. (21,22)
With the unprecedented hike in incidence, India has become the global epicenter of the pandemic. (23) Socioeconomic inequities, in addition to the steady demand, hinder equitable access to healthcare resources. While the financially sophisticated manage to procure the resources needed, people of lower socioeconomic status struggle to access essential care and life support. Psychosocial impacts of the pandemic and lockdown aside, the prevalence of stigma among society delay diagnosis and impede disease control. The discrimination is seen directed primarily at lower socioeconomic groups, people who have recovered from COVID-19, and healthcare workers. (24)
With the second wave witnessing the pandemic’s peak, the incidence of Long COVID is also expected to surge. There exists a severe deficit of research into the long-term effects and rehabilitation after the acute infective phase. In the absence of active rehabilitative measures, the country could face another wave soon.
Rehabilitation, at its core, encompasses assessment, monitoring, prevention, intervention, supervision, education, consultation, and counseling. (31) Telerehabilitation refers to the use of distance communication technologies to satisfy the components of rehabilitation. Evidence suggests that telerehabilitation is a feasible alternative for physical rehabilitation in stroke patients, physiotherapy, and neurorehabilitation as studied before the pandemic. (32-34) Studies have also shown comparable clinical outcomes and patient satisfaction with cost-effectiveness in telerehabilitation compared to conventional methods. (35-37) With physical access being restricted in light of the pandemic, telerehabilitation becomes essential for the rehabilitative care continuum.
The global rehabilitation alliance has suggested that rehabilitative care be given to COVID-19 patients as early as the acute phase. It is to be continued in early, late post-acute, and long-term phases. (38) Remote assessment of the long COVID patients, followed by intervention and long-term monitoring while providing psychological support, constitute the foundation of telerehabilitation for COVID-19. Telerehabilitation has also been found viable for inpatients suffering from COVID-19 by a study conducted in the European population. (39)
Many teleconsultation services already exist in India, like the one by the Ministry of Health and Family Welfare, esanjeevni platform. (40) However, telerehabilitation services have not been conscientiously implemented. The formidable disease load in India makes emphasizing telerehabilitation dubious. However, an epidemic of long COVID would be imminent if adequate measures are not taken on time. An exemplary setup of telerehabilitation for visually challenged individuals during the pandemic at All India Institute of Medical Sciences, Delhi, India, provides an optimistic outlook of the future of telerehabilitation in India. (41)
Due to the unforeseen COVID surge in India, dealing with the staggering load of active cases and resource distribution is given paramount importance. With the healthcare system being overwhelmed and understaffed, the handling of rehabilitation becomes nearly improbable. With society in survival mode, people’s perception of rehabilitation also needs significant improvement. There is a dire need for establishing, implementing, and centralizing a Telerehabilitation system in India.
The authors suggest developing a web portal that serves as a repository for Long COVID and a centralized Telerehabilitation tool. Building a centralized repository helps enhance record-keeping and tracking symptoms of long COVID. Two pathways are proposed for the data compilation-the first, passive, and the second, active data collection. In the passive pathway, a reporting system shall be developed through which the survivors and physicians will report symptoms of long COVID. The inputs can undergo thorough screening before being submitted to the repository. Self-reporting of symptoms is observed to make significant revelations about the disease and, therefore, predict the rehabilitation needs of the patients. (42) The second active pathway involves post-hospitalization follow-up of COVID-19 survivors by a follow-up team. With the physicians engaged in acute care, medical students can be a potential alternative. The team could include medical (MBBS) and nursing students who have been trained in medical history taking and COVID-19 specific follow-up.
The patients will be contacted by the team via telecommunication and enquired about their symptoms if any. The database will then be updated. The information thus collected could help establish rehabilitation guidelines as well as in pursuing clinical training of medical students. Figure 1 demonstrates the algorithm of the telerehabilitation portal.
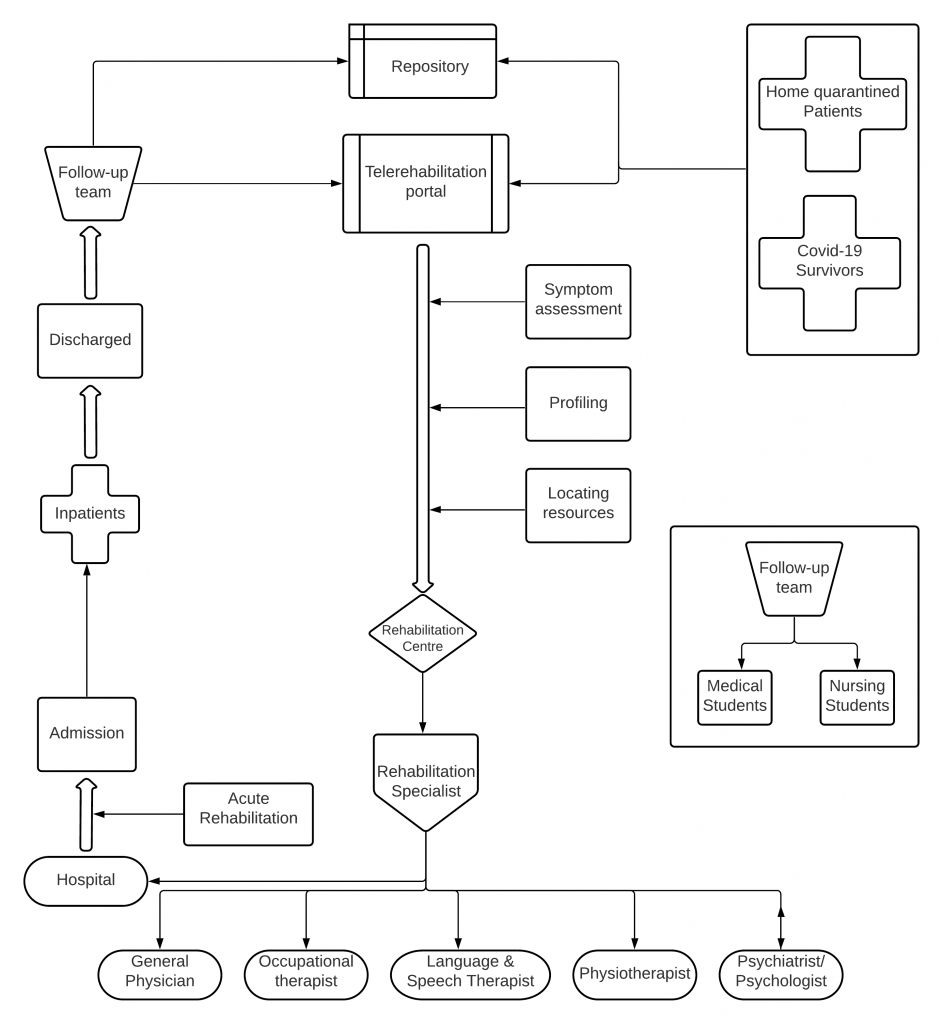

Tele rehabilitation not only integrates safety (social distancing) in providing healthcare interventions but also helps lessen the burden on the physicians. The patients/survivors, through the portal, can access the rehabilitation specialist they require in the nearest rehabilitation center. Once the patient/survivor enters the details, their symptoms are assessed, profiled, and redirected to a nearby rehabilitation center with required resources.
Several challenges could arise in the proper implementation of the suggestion. At the outset, medical and nursing students can only be employed after adequate training to handle the follow-up of COVID-19 patients. Secondly, lack of awareness regarding rehabilitation in India might pose an initial barrier; however, with active campaigning both by the private and government sector, this can be solved. Given the technical readiness of the target demographic, the average time of implementation can be longer than expected.
Due to the impact of the ongoing coronavirus pandemic and its unpredictable course, it is anticipated that many patients will have some residual symptoms that need some rehabilitation support. Physicians should be well informed about the latest developments and guidelines to provide this support. The proposed protocol includes a repository that helps centralize the data on long COVID, thereby helping the physicians stay up to date. The telerehabilitation portal ensures providing rehabilitative care without actively burdening the healthcare system. It also helps raise awareness on the necessity and importance of rehabilitation in COVID-19 care. As the pandemic grows in leaps and bounds, the healthcare agencies across the world and India should begin taking care of the rehabilitative needs of the COVID-19 survivors with residual symptoms with adequate data collection systems and, as a result, practice cost-efficient and proper evidence-based medicine.
BCPHR.org was designed by ComputerAlly.com.
Visit BCPHR‘s publisher, the Boston Congress of Public Health (BCPH).
Email [email protected] for more information.
Click below to make a tax-deductible donation supporting the educational initiatives of the Boston Congress of Public Health, publisher of BCPHR.![]()
© 2025-2026 Boston Congress of Public Health (BCPHR): An Academic, Peer-Reviewed Journal
All Boston Congress of Public Health (BCPH) branding and content, including logos, program and award names, and materials, are the property of BCPH and trademarked as such. BCPHR articles are published under Open Access license CC BY. All BCPHR branding falls under BCPH.
Use of BCPH content requires explicit, written permission.